Development of 3D vision software for medical training: trainees’ assessment of learning effectiveness
Desarrollo de software de visión 3D para la formación médica: evaluación de la eficacia del aprendizaje por parte de los alumnos
Manuela Martín Izquierdoa, Marcelo F. Jiménez Lópezaa, b, Alberto Prats-Galinoa, c, Juan A. Juanes Méndeza, d(*)
a Group VisualMed Systems. University of Salamanca.
Radiodiagnosis Service. Salamanca University Hospital. Spain
https://orcid.org/0000-0002-5562-3550mmimhp@gmail.com
b Instituto de Ciencias de la Educación University of Salamanca. Thoracic Surgery Service. Salamanca University Hospital. Spain
https://orcid.org/0000-0003-2184-0159mfjl@usal.es
c Laboratory of Surgical NeuroAnatomy (LSNA), Faculty of Medicine and Health Sciences. University of Barcelona. Spain
https://orcid.org/0000-0002-2710-6433aprats@ub.edu
d Instituto de Ciencias de la Educación University of Salamanca. Department of Human Anatomy. Faculty of Medicine. University of Salamanca. Spain
https://orcid.org/0000-0003-2749-3426jajm@usal.es
ABSTRACT
This article presents a technological development that makes it possible to visualize the anatomy of the respiratory system in three dimensions (3D), embedded in magnetic resonance (MRI) serial sections in the coronal, sagittal, and axial planes. The relevant anatomical regions were delimited in the MRI sections with commercial software. This paper presents the opinion of students who have taken the subject of Human Anatomy on the use and management, for their learning, of interactive technological resources for the three-dimensional visualization of body structures. After the students had used a computer application developed by our working group, a satisfaction survey was presented to them to assess their interest in autonomous learning using this technological development. After the results were obtained, we can deduce that the students who used the interactive 3D vision application highlighted its high teaching value, as it is easy to use due to its intuitive interface. They considered this technological teaching resource to have a high degree of satisfaction in their teaching-learning process, given its 3D visual and dynamic nature. For all these reasons, the students considered using these resources to be very useful in their medical training, as opposed to the classic static anatomical atlases. Over the last few years, new technologies have significantly increased the number of applications in diagnostic imaging and medical training, specifically in the medical training in anatomy.
Keywords:
technology, 3D vision software, autonomous learning, human anatomy
RESUMEN
Este artículo presenta un desarrollo tecnológico que permite visualizar la anatomía del aparato respiratorio en tres dimensiones (3D), incrustada en secciones seriadas de resonancia magnética (RM) en los planos coronal, sagital y axial. Las regiones anatómicas relevantes se delimitaron en las secciones de RM con software comercial. Este trabajo presenta la opinión de estudiantes que han cursado la asignatura de Anatomía Humana sobre el uso y manejo, para su aprendizaje, de recursos tecnológicos interactivos para la visualización tridimensional de estructuras corporales. Tras la utilización por parte del estudiantado de esta aplicación informática desarrollada por nuestro grupo de trabajo, se les presentó una encuesta de satisfacción para valorar el grado de interés y aprendizaje autónomo utilizando este tipo de desarrollos tecnológicos. Tras los resultados obtenidos, podemos deducir que los alumnos que utilizaron la aplicación interactiva de visión 3D destacaron su alto valor didáctico, ya que es fácil de utilizar debido a su interfaz intuitiva. Consideraron que este recurso tecnológico didáctico tiene un alto grado de satisfacción en su proceso de enseñanza-aprendizaje, dado su carácter visual 3D y dinámico. Por todo ello, los alumnos consideraron muy útil el uso de estos recursos en su formación médica, frente a los clásicos atlas anatómicos estáticos. En los últimos años, las nuevas tecnologías han aumentado significativamente el número de aplicaciones en el campo del diagnóstico por imagen y la formación médica, y más concretamente en el campo de la anatomía.
Palabras clave:
tecnología, software Visión 3D, aprendizaje autónomo, anatomía humana
1. Introduction
Macroscopic anatomy is one of the pillars of training in medicine and other health sciences. Traditional teaching methods of human anatomy involve textbooks, atlases, and cadaver dissection (Preim & Saalfeld, 2018).
The three-dimensional view (3D) of the human body architecture represents a significant advance in the teaching-learning process in human anatomy and in the area of clinical diagnosis (Arraez-Aybar et al., 2010; Asensio Romero et al., 2018; Mavar-Haramija et al., 2015; Prats-Galino et al., 2015; Shin et al., 2013).
The advances in medicine have been made hand in hand with advances in imaging techniques and the appearance of new technologies that make clinical practice easier, promoting the safety of practitioners and patients alike. The great anatomical detail provided by images acquired through different current radiological techniques such as multidetector computed tomography (CT) and magnetic resonance imaging (MRI) are expanding the horizon of medical sciences in general and human anatomy in particular. A specialized software application that includes the graphic workstations from the Radiodiagnosis Services encodes the information in a standard DICOM format (Digital Imaging and Communications in Medicine) and makes it possible to observe a virtual volume on the computer screen in different planes that can be processed digitally.
Applying volume rendering techniques to these images makes it possible to generate a 3D volume that can be transferred between devices (Malmberg et al., 2017; Perandini et al., 2010). The post-processing of radiological images and the 3D reconstruction of their anatomical structures have improved the visualization of the body morphology and made it possible to diagnose different disorders.
The objective of this study is to present a technological tool for the 3D visualization of the main anatomical structures in the respiratory system, embedded in MRI sections in the three spatial planes (axial, coronal, and sagittal) to make it easier to observe and learn from them, and to improve the knowledge of the configuration of these structures and topographic relations.
2. Materials and Methods
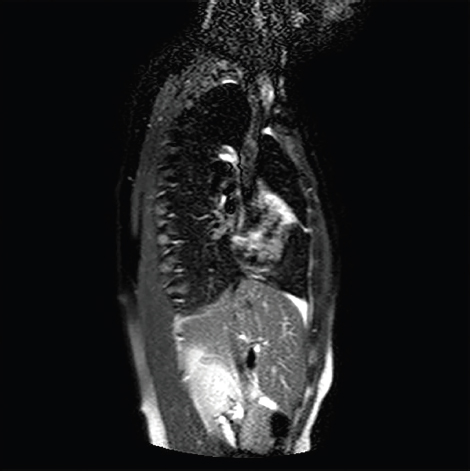
The study used MRI devices at 1.5 Teslas (Signa Horizon. General Electric -GE-) and 3 Teslas (Vida. Siemens) to obtain serial sections in the three spatial planes (Figures 1, 2, and 3).
Figure 1. Axial MRI section of the thorax.
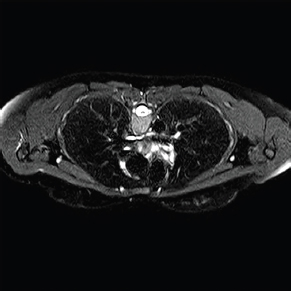
Figure 2. Coronal or frontal MRI section of the thorax.
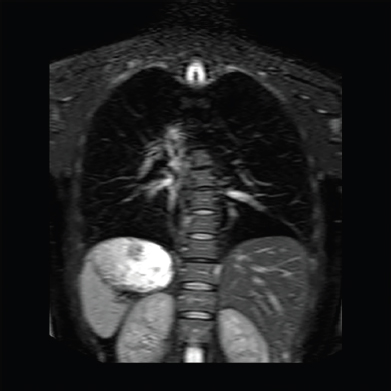
Figure 3. Sagittal MRI section of the thorax.
High-resolution T1- and T2-weighted images were obtained with an established protocol (Loc. SSFSE, Coronal T2 FSE, 2D FIESTA, Axial T2 PROPELLER FSE), as well as EPI DWI sequences, and a dynamic study was conducted before and after gadolinium administration with LAVA sequences (SPGR 3D).
The dynamic study was conducted using the Dixon technique (in-phase/out-of-phase sequences) with GRE sequences (shorter than SE sequences), which is easier to perform when the patient is suspending respiration.
Afterward, the images were registered and re-dimensioned in the three planes to obtain aligned volumes with 1-mm isotropic voxels. The anatomical regions of interest, corresponding to the main structures of the respiratory system, were determined manually with the software 3D Amira© (Mercury/TGS-Europe, Inc.). The segmentation and delimitation of the ROIs (regions of interest) involved the subdivision of each anatomic image into homogeneous regions; that is, the perimeter of a specific structure to be modeled in three dimensions was selected. The software allowed the researchers to improve the surfaces, remove artifacts, select a specific part of the segmentation, or scale the model, among other functions.
The 3D modeling process described above is based on the serial sections in DICOM format that generate the 3D models of the structures of the respiratory system. Although Amira© was primarily used, other open-source software applications were used to render volumes or surfaces, including Osirix, Horos, 3D Slicer, and InVesalius.
The manual segmentation process was very demanding and time-consuming since it was performed individually for each dataset and under the supervision of an anatomical radiologist (Figure 4). The algorithm used was Marching Cubes, which makes it possible to extract a polygonal mesh of an isosurface from voxels. In sum, the different anatomical surface models of triangular mesh were generated from the ROIs.
Figure 4. The process of manual segmentation limits the different regions of interest.
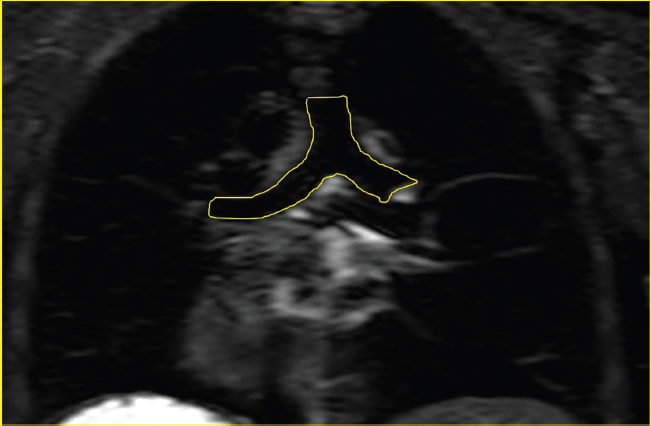
The reconstruction of the trachea and the main bronchi was conducted with ROIs that included the lumen and the adjacent tissue due to the high intensity of the tissue (Figure 4). The lower threshold was set at zero, and the upper threshold was determined based on the average noise level of the signal plus twice its standard deviation. The diaphragm, ribs, and spine have been reconstructed as reference anatomical structures.
Both the MRI sections and the 3D anatomical models generated were visualized in a software application specifically developed by our team. This software represents graphic images in real-time in any spatial orientation, and the images can be stored in bitmap format. It was developed following market standards to make it compatible with most computer devices and the different versions of the Windows OS used by most of the students and universities in Spain. The application was programmed in Visual C++, which, as an integrated development environment, made it possible to implement object-oriented programming (OOP) with the programming languages C, C++, and C++/CLI, together with Windows software development kit (SDK), also known as an application programming interface (API).
Satisfaction surveys were carried out with a group of medical students (n=35) to assess and determine the degree of teaching usefulness of this computer tool, considering a sufficiently representative number to obtain a sample to guide us on the students' satisfaction with the technological development presented. All the students had previous knowledge of the subject and had passed the human anatomy course on splacnology before carrying out the satisfaction survey.
The survey focused exclusively on the computer development itself, trying to assess the effectiveness and satisfaction of the users who used the teaching program on the anatomy of the respiratory apparatus, with three-dimensional views of these structures embedded in radiological sections of magnetic resonance imaging.
The data were processed with Microsoft Excel spreadsheet software, which allowed us to analyze and process all the survey data and present the different graphs.
3. Results
The MRI technique allowed the team to assess the morphology of the different tissue types, thanks to the generated signal intensities. Different sequences (T1 and T2) made it possible to modify the signal intensity values in the segmentation procedure, representing differences in the tissue’s physical and chemical composition.
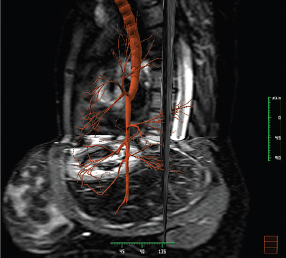
The thoracic cavity MRI technique has become the method of choice for the morphological study of the structures of the respiratory system because it clearly shows the contrast between fat, muscle tissue, bone structures, and viscera, which also presents an adequate view of the anatomical integrity of the thoracic cavity. Therefore, the analysis of the thorax with MRI on different spatial planes provides excellent information on the morphology of these structures (Figure 5).
Figure 5. View of 3D structures of the respiratory system embedded in MRI sections.
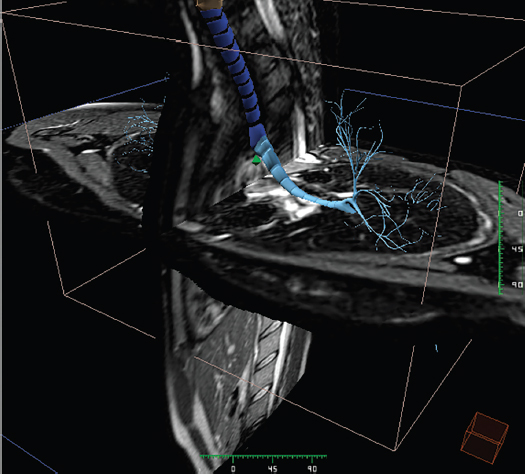
The central airways are shown as structures without a signal due to the air inside them. Their anatomical location can differentiate them from the vessels (Figure 6). In the blood vessels, the fast blood flow creates a lack of signal inside the vascular structures that can be easily distinguished from the typical hyperintensity of the surrounding fat tissue.
Figure 6. 3D view of the bronchial tree embedded in MRI sections.
At the cervical level, the larynx is delimited by the laryngeal cartilages (Figure 6), which are ossified at 25 years of age and present as hypointense cortical bone in T1- and T2-weighted sequences, with a medullary cavity that contains fat and is hyperintense in T1-weighted sequences.
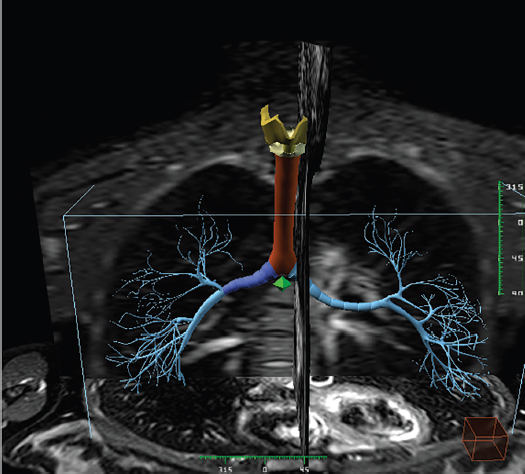
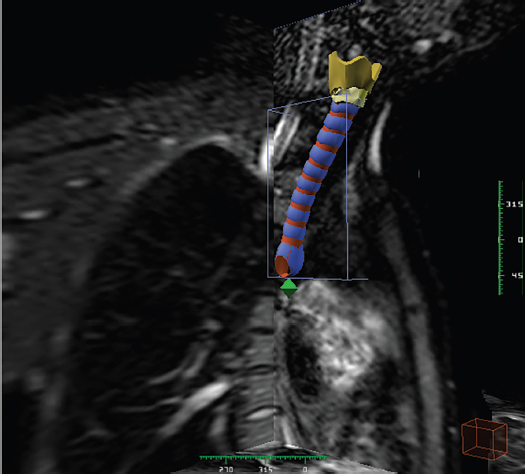
In the thoracic study, all sequences show the trachea as hypointense (Figure 7). The tracheal rings show an intermediate signal compared to the fat surrounding them, and their wall can be perfectly delimited. The sectional images show a straight course, 10 to 12 cm long, with the upper end at the 6th or 7th cervical vertebra level and its lower end reaching the 3rd or 4th thoracic vertebra (Figure 7 and Figure 8). It is surrounded by a layer of abundant loose cell tissue, like a serous membrane. The frontal part of the trachea is next to the isthmus of the thyroid gland, which covers its first 2 or 3 rings. The back of the trachea faces the esophagus. The tracheal bifurcation leads to the main bronchi in the middle mediastinum. This bifurcation is at the level of the 3rd to 5th thoracic vertebrae. The bronchi are headed downwards, outwards, and backward until they reach the hila of the right and left lungs, respectively. Their structure is similar to the trachea.
Figure 7. View of a 3D reconstruction of the laryngeal cartilages, trachea, and main bronchi.
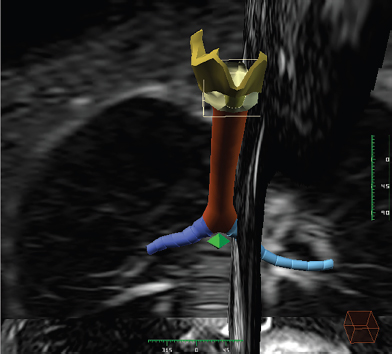
Figure 8. View of a 3D reconstruction of the laryngeal cartilages and trachea.
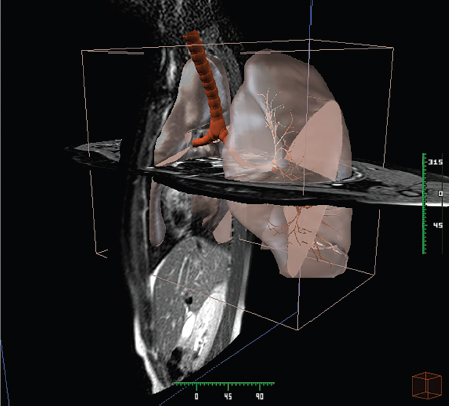
When the main bronchi enter through the hilum of each lung, they are divided into intrapulmonary lobar bronchi, which branch out asymmetrically inside the pulmonary parenchyma and are very difficult to delimit and segment (Figure 9). Therefore, in this study, the intrapulmonary bronchi were classified as ventral, distributed throughout the external and anterior regions of the lungs; dorsal, heading backward to occupy the posterior regions; and antero-internal, distributed in the internal and lower part of both lungs. These divisions correspond to each of the pulmonary lobes.
Figure 9. View of the bronchial tree embedded in MRI sections on the three spatial planes.
The pulmonary parenchyma creates a low signal due to its low proton density. The 3D reconstruction of these structures reveals a convex semicone projecting outwards whose base rests on the diaphragm and whose vertex points to the superior thoracic aperture and projects cranially between 25 and 30 mm (Figure 10 and Figure 11).
Figure 10. Frontal view of the pulmonary parenchyma with a transparent bronchial tree inside.
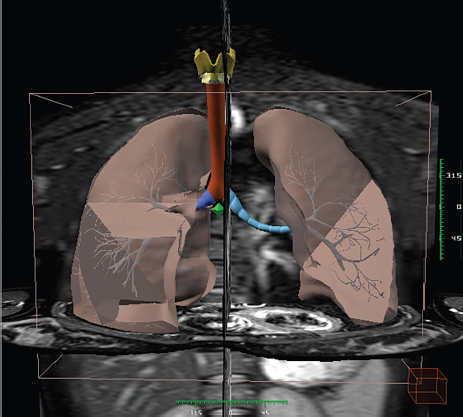
Figure 11. Lateral view of the pulmonary parenchyma with a transparent bronchial tree inside.
The vascular structures of the mediastinum show an intermediate signal in SE, T1, and T2 sequences (“black blood”) due to the movement of the blood and the protons in it, and they are hyperintense in GRE sequences (“white blood”).
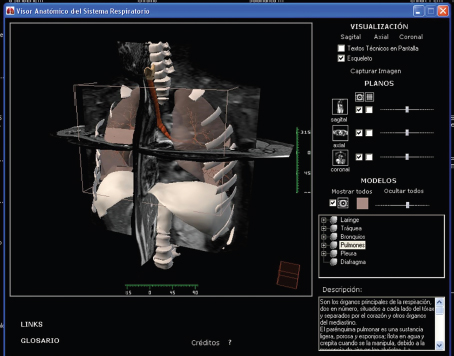
To visualize and interact with the radiological images and the 3D anatomical structures, a computer application was developed for Windows platforms and encoded with the software Visual C++ (see Materials and Methods section). The user interface is very intuitive and user-friendly (Figure 12).
Figure 12. Anatomic viewer for the visualization of 3D images. The different options to view and interact with the images can be seen (zoom, color, anatomical description, etc.).
The results obtained from the survey on evaluating the radiological anatomy software of morphological structures that form part of the respiratory system show positive data regarding satisfaction and learning through this technological tool.
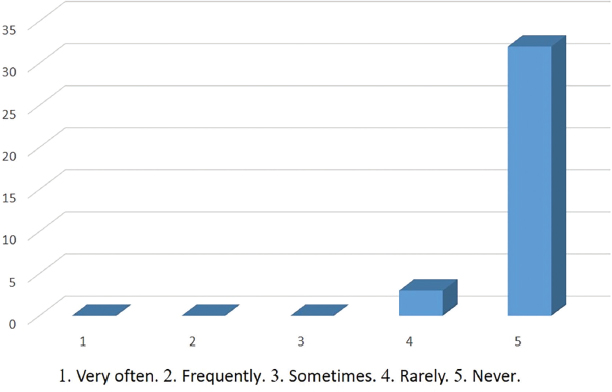
The students highlighted that the software developed positively, with 43% of those surveyed indicating that it was easy to install, 54% straightforward (Figure 13), and practically 100% of users indicated that the application never or rarely crashes (Figure 14).
Figure 13. How was the software installation?
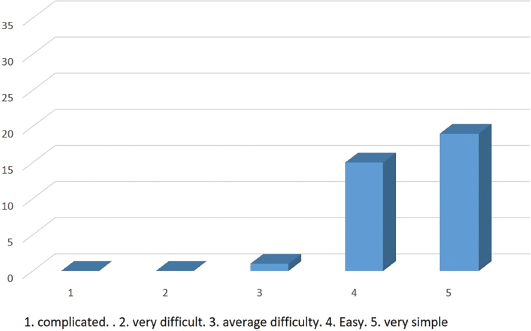
Figure 14. How often does the software crash?
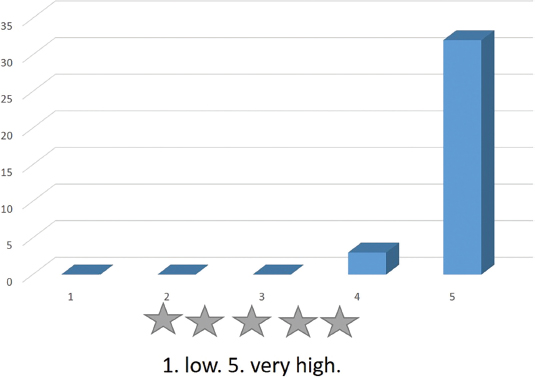
Navigation through the program is very intuitive (Figure 15). Moreover, the 3D view of the anatomical structures facilitates their understanding and study (Figure 16).
Figure 15. Navigation through the program is very intuitive and presents a methodological development that motivates learning in an agile and simple way.
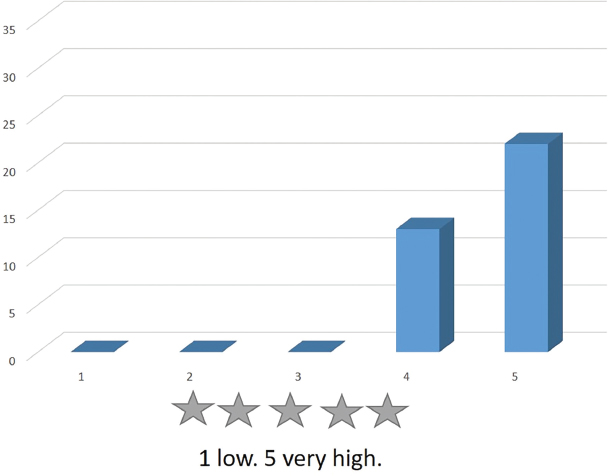
Figure 16. The three-dimensional view of the structures of the respiratory system facilitates a better understanding and analysis of each one of them.
From the teaching point of view, it is highly valued as a good complementary didactic resource for study. A good group of respondents indicated that this tool is a suitable medium that surpasses many static anatomic-radiological atlases. The visual presentation of the contents is beautiful and, therefore, highly valued by the students.
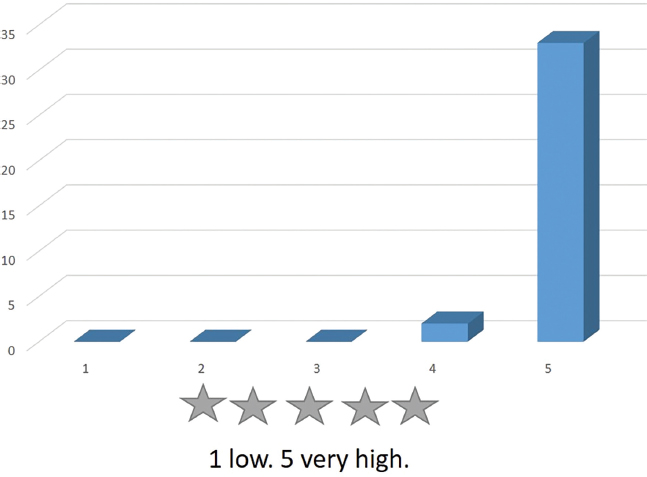
The brief explanatory comments on the anatomical structures displayed are well appreciated (Figure 17), and the program interface is very intuitive and user-friendly, a response given by almost 100% of users (Figure 18).
Figure 17. The short explanatory comments on the screen help you to understand the anatomy of the respiratory system better and to reinforce your knowledge.
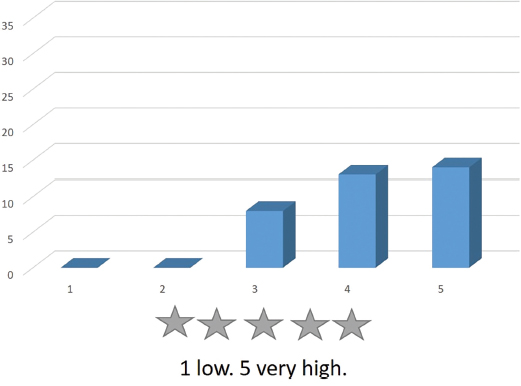
Figure 18. The program interface is intuitive and user-friendly.
After the data is obtained, we can point out that using 3D visualization technological environments for training in human anatomy constitutes a new source of opportunities for the teaching-learning processes. They offer a three-dimensional representation of organs and structures, allowing them to be viewed from different angles and distances, facilitating understanding of complex concepts. They are intuitive and appealing to students, providing further motivation for student learning.
4. Discussion
Despite the advances in imaging unit technology and their availability, the use of the thoracic MRI technique has not been sufficiently developed, and few studies have analyzed the structures of the respiratory system from a morphological perspective. On the contrary, other techniques, such as TC, are the predominant method in this type of exploration. Therefore, the 3D reconstruction of anatomical structures embedded in the volumetric data of magnetic resonance images is an obvious and intuitive form of morphological analysis because a simple individual exam of its different sections makes it possible to quickly understand the group of anatomical elements that make up the respiratory system. The soft tissue characterization in non-cardiovascular and non-musculoskeletal thoracic MRI studies has been considered impractical due to its challenges, such as respiratory movement, cardiac movement, vascular pulsation, air susceptibility, and low lung signal. However, the current advances in MR imaging have made it possible to obtain good-quality MR images of the thorax that are useful for diagnosis, although the literature on subspecialized practices of thoracic MRI is limited (Abildgaard et al., 2010; Gamsu et al., 1983; Thompson & Stanford, 2000; Venkatesh et al., 2011; Webb et al., 1984).
Our technological innovation is a suitable method to visualize 3D structures with the sectional MR image as a reference in the three spatial planes, which makes it easier to conduct an anatomical assessment of these structures and to use the advanced graphic power provided by computers nowadays.
Currently, it is accepted that the reconstruction and 3D visualization of anatomical structures from any part of the body provide more accurate and valuable information for clinical diagnosis, and they also lead to more dynamic and visual learning of the body anatomy. For these reasons, significant efforts have been made over the last years to automatize the analysis of 3D medical images to support diagnostic tasks (González-Izard et al., 2020).
The 3D reconstruction of anatomical structures of the human body also makes it possible to develop virtual learning environments through interactive visualization with stereoscopic glasses (González-Izard et al., 2018). Therefore, several technological developments have recently emerged that apply these tools to the fields of human anatomy, radiology, clinical medicine, and surgery (AbouHashem et al., 2015; McMenamin et al., 2014; Olabarriaga & Smeulders, 2001). The collaboration of anatomists, radiologists, and surgeons is an excellent line of work that faithfully reconstructs the morphological structures of the body.
Many authors agree that any 3D visualization mode (computer-generated 3D images, stereoscopic vision with virtual reality, and augmented reality techniques) applied to teaching human anatomy is very useful in the learning process (Abildgaard et al., 2010; Adams et al., 2019; Blum et al., 2012; Boonbrahm et al., 2018; Johnson et al., 2016; Robison et al., 2011; Tabernero Rico et al., 2017).
5. Conclusions
Thoracic MRI provides detailed images of different structures of the thoracic cavity. Using technological resources for the 3D representation of medical images improves spatial perception and anatomical understanding. It makes it possible to create teaching material related to radiological images, such as MRIs.
One of the challenges of medical training in this millennium is adapting new technologies to the teaching and learning process. This article shows the potential of 3D anatomy to promote the general use of these technological resources in medical teaching and the clinical field. 3D modeling and 3D technologies have shown that they are potent tools for learning human anatomy and clinical diagnosis. Many applications are being discovered in medical sciences, particularly in surgical approaches. However, deep technical knowledge and highly complex software are required to develop these technological environments for 3D visualization.
Implementing these new technological resources to visualize body structures embedded in serial sections of radiological images, such as MRI, in medical training is an advance in the systems to teach and learn human anatomy. The use of 3D technology presents several advantages over the traditional 2D models in studying anatomical structures. Learning and studying 3D anatomical models such as the one developed by our team makes it possible to understand the respiratory system's structures better.
The students who handled the computer tool considered it a very innovative design that facilitates studying, understanding, and learning anatomical structures. Introducing these didactic technological tools in teaching considerably enriches the teaching-learning process. Learning by interacting with information motivates and gives students an active attitude for autonomous and meaningful learning.
Authors’ contribution
Manuela Martín Izquierdo: Conceptualization. Segmentation of radiological images. Drafting, revision, and editing.
Marcelo F. Jiménez López: Conceptualization, 3D image analysis, Drafting, proofreading and editing.
Alberto Prats Galino: Review of anatomical structures. Computer development. Drafting, proofreading, and editing.
Juan A. Juanes Méndez: Revision of anatomical structures. Computer development Drafting, proofreading, and editing.
References
Abildgaard, A., Witwit, A. K., Karlsen, J. S., Jacobsen, E. A., Tennoe, B., Ringstad, G., Due-Tønnessen, P. (2010) An autostereoscopic 3D display can improve visualization of 3D models from intracranial MR angiography. International Journal of Computer Assisted Radiology and Surgery. 5(5), 549–554. https://doi.org/10.1007/s11548-010-0509-5
AbouHashem, Y., Dayal, M., Savanah, S, & Štrkalj, G. (2015). The application of 3D printing in anatomy education. Medical Education Online, 20(1). https://doi.org/10.3402/meo.v20.29847
Adams, H., Shinn, J., Morrel, W. G., Noble, J., & Bodenheimer, B. (2019). Development and evaluation of an immersive virtual reality system for medical imaging of the ear. Proceedings Volume 10951, SPIE Medical Imaging 2019: Image-Guided Procedures, Robotic Interventions, and Modeling (San Diego, CA, USA, 8 March 2019). https://doi.org/10.1117/12.2506178
Arraez-Aybar, L. A., Sanchez-Montesinos, I., Mirapeix, R.-M., Mompeo-Corredera, B., & Sanudo-Tejero, J.-R. (2010). Relevance of human anatomy in daily clinical practice. Annals of Anatomy-Anatomischer Anzeiger, 192(6), 341-348. https://doi.org/10.1016/j.aanat.2010.05.002
Asensio Romero, L., Asensio Gómez, M., Prats-Galino, A., & Juanes Méndez, J. A. (2018). 3D Models of Female Pelvis Structures Reconstructed and Represented in Combination with Anatomical and Radiological Sections—Journal of Medical Systems, 42(3), 37. https://doi.org/10.1007/s10916-018-0891-z
Blum, T., Kleeberger, V., Bichlmeier, C., & Navab, N. (2012). mirracle: Augmented Reality in-situ visualization of human anatomy using a magic mirror. In 2012 IEEE Virtual Reality Workshops (VRW) (Costa Mesa, CA, USA, 4-8 March 2012) (pp. 169-170). IEEE. https://doi.org/10.1109/VR.2012.6180934
Boonbrahm, P., Kaewrat, C., Pengkaew, P., Boonbrahm, S., & Meni, V. (2018). Study of the Hand Anatomy Using Real Hand and Augmented Reality. International Journal of Interactive Mobile Technologies, 12(7), 181-190. https://doi.org/10.3991/ijim.v12i7.9645
Gamsu, G., Webb, W. R., Sheldon, P., Kaufman, L., Crooks, L. E., Birnberg, F. A., Goodman, P., Hinchcliffe, W. A., & Hedgecock, M. (1983). Nuclear magnetic-resonance imaging of the thorax. Radiology, 147(2), 473–480. https://doi.org/10.1148/radiology.147.2.6836125
González-Izard, S., Juanes-Méndez, J. A., García-Peñalvo, F. J., Gonçalvez-Estella, J. M., Sánchez-Ledesma, M. J., & Ruisoto-Palomera, P. (2018). Virtual Reality as an Educational and Training Tool for Medicine. Journal of Medical Systems, 42, 50. https://doi.org/10.1007/s10916-018-0900-2
González-Izard, S., Sánchez Torres, R., Alonso Plaza, Ó., Juanes-Méndez, J. A., & García-Peñalvo, F. J. (2020). Nextmed: Automatic Imaging Segmentation, 3D Reconstruction, and 3D model Visualization Platform Using Augmented and Virtual Reality. Sensors, 20(10), 2962. https://doi.org/10.3390/s20102962
Johnson, S., Jackson, B., Tourek, B., Molina, M., Erdman, A. G., & Keefe, D. F. (2016). Immersive Analytics for Medicine: Hybrid 2D/3D Sketch-Based Interfaces for Annotating Medical Data and Designing Medical Devices. In Proceedings of the 2016 ACM Companion on Interactive Surfaces and Spaces (Niagara Falls, Ontario, Canada, November 6-9, 2016) (pp. 107–113). Association for Computing Machinery. https://doi.org/10.1145/3009939.3009956
Malmberg, F., Nordenskjold, R., Strand, R., & Kullberg, J. (2017). SmartPaint: a tool for interactive segmentation of medical volume images. Computer Methods in Biomechanics and Biomedical Engineering-Imaging and Visualization, 5(1), 36-44. https://doi.org/10.1080/21681163.2014.960535
Mavar-Haramija, M., Prats-Galino, A., Juanes Méndez, J. A., Puigdelivoll-Sánchez A., & de Notaris, M. (2015). Interactive 3D-PDF Presentations for the Simulation and Quantification of Extended Endoscopic Endonasal Surgical Approaches. Journal of Medical Systems, 39(10), 127. https://doi.org/10.1007/s10916-015-0282-7
McMenamin, P. G., Quayle, M. R., McHenry, C. R., & Adams, J. W. (2014). The Production of Anatomical Teaching Resources Using Three-Dimensional (3D) Printing Technology. Anatomical Sciences Education, 7(6), 479–486. https://doi.org/10.1002/ase.1475
Olabarriaga, S. D., & Smeulders, A. W. M. (2001). Interaction in the segmentation of medical images: A survey. Medical Image Analysis, 5(2), 127-142. https://doi.org/10.1016/S1361-8415(00)00041-4
Perandini, S., Faccioli, N., Zaccarella, A., Re, T., Mucelli, R. P. (2010). The diagnostic contribution of CT volumetric rendering techniques in routine practice. The Indian Journal of Radiology & Imaging, 20(2), 92-97. https://doi.org/10.4103/0971-3026.63043
Prats-Galino, A., Reina, M. A., Mavar-Haramija, M., Puigdellivol-Sánchez, A., Juanes Méndez, J. A., & de Andrés, J. A. (2015). 3D Interactive Model of Lumbar Spinal Structures of Anesthetic Interest. Clinical Anatomy, 28(2), 205-212. https://doi.org/10.1002/ca.22479
Preim, B., & Saalfeld P. (2018). A survey of virtual human anatomy education systems. Computers & Graphics, 71, 132-153. https://doi.org/10.1016/j.cag.2018.01.005
Robison, R. A., Liu, C. Y., & Apuzzo, M. L. J. (2011). Man, Mind, and Machine: The Past and Future of Virtual Reality Simulation in Neurologic Surgery. World Neurosurgery, 76(5), 419-430. https://doi.org/10.1016/j.wneu.2011.07.008
Shin, D. S., Jang, H. G., Hwang, S. B., Har, D.-H., Moon, Y. L., & Chung, M. S. (2013). Two-dimensional sectioned images and three-dimensional surface models for learning the anatomy of the female pelvis. Anatomical Sciences Education, 6(5), 316-323. https://doi.org/10.1002/ase.1342
Tabernero Rico, R. D., Juanes Méndez, J. A., & Prats Galino, A. (2017). New Generation of Three-Dimensional Tools to Learn Anatomy. Journal of Medical Systems, 41(5), 88. https://doi.org/10.1007/s10916-017-0725-4
Thompson, B. H., & Stanford, W. (2000). MR imaging of pulmonary and mediastinal malignancies. Magnetic resonance imaging clinics of North America, 8(4), 729–39. https://doi.org/10.1016/S1064-9689(21)00640-1
Venkatesh, V., Verdini, D., & Ghoshhajra, B. (2011). Normal Magnetic Resonance Imaging of the Thorax. Magnetic Resonance Imaging Clinics of North America, 19(3), 489-506. https://doi.org/10.1016/j.mric.2011.05.014
Webb, W. R., Gamsu, G., Stark, D. D., & Moore, E. H. (1984). Magnetic-resonance imaging of the normal and abnormal pulmonary hila. Radiology, 152(1), 89-94. https://doi.org/10.1148/radiology.152.1.6729141
(*) Autor de correspondencia / Corresponding author