eISSN 2444-7986
DOI: https://doi.org/10.14201/orl.28188
ORIGINAL ARTICLE
CHARACTERIZATION OF PAIN IN THE FIRST TWO WEEKS AFTER TONSILLECTOMY IN CHILDREN 3 TO 8 YEARS OLD. A PILOT STUDY
Caracterización del dolor en las primeras dos semanas tras amigdalectomía en niños de 3 a 8 años. Un estudio piloto
Juan Manuel GRANADOS-SITGES  1; Alex RAMIREZ-ROSA
1; Alex RAMIREZ-ROSA  1; Jose GRANELL
1; Jose GRANELL  1,2; Javier HERNÁNDEZ-CALVÍN
1,2; Javier HERNÁNDEZ-CALVÍN  2, 3
2, 3
1 Servicio de Otorrinolaringología. Hospital Universitario Rey Juan Carlos. Móstoles. Madrid. España.
2 Facultad de Ciencias Biomédicas y de la Salud. Universidad Europea de Madrid. Villaviciosa de Odon. Madrid. España.
3 Servicio de Otorrinolaringología. Hospital Universitario Quirónsalud Madrid. Pozuelo. Madrid. España.
Correspondence: juan.granadoss@hospitalreyjuancarlos.es
Reception date: January 17, 2022
Date of Acceptance: February 10, 2022
Publication date: February 15, 2022
Date of publication of the issue: September 30, 2022
Conflict of interest: The authors declare no conflicts of interest
Images: The authors declare that the images have been obtained with the permission of the patients
Rights policy and self-archive: the self-archive of the post-print version (SHERPA / RoMEO) is allowed
License CC BY-NC-ND. Creative Commons Attribution-Noncommercial-NoDerivate Works 4.0 International
University of Salamanca. Its commercialization is subject to the permission of the publisher
SUMMARY: Introduction and objective: To study the pain in children is a challenge. Tonsillectomy is a very common and painful surgical procedure in which there are still barriers to warrant an adequate pain management. The purpose of this study is to characterize the pain after surgery in children between 3 and 8 years-old who underwent tonsillectomy. Method: We performed a descriptive, observational and prospective study in children aged 3 to 8 who underwent tonsillectomy. The data collection was made through a pain questionnaire based in the intensity of pain from 0-10 in the Wong Baker scale (based on drawn faces). Parents also fulfilled other questions about the days that the children could not attend the school and the working days that the parents themselves lost. The analgesic treatment that each child received was also recorded. Results: Twenty-nine patient were included, 14 girls and 15 boys with a median age of 4. The highest level of pain was found the second day with a median value of 3,0. This second day was so chosen to compare the level of pain between indications. The median pain was 3,0 when it was for obstructive disease, but 4,0 when obstruction was associated with facial growth disorders. Children lost a median of 8 days at school and their parents 2 days at work each one. Discussion: Our limited data suggest that the long-term side effects of the upper airway obstruction due to tonsillar hypertrophy like disorders of facial growth made the surgery more painful and that the pain had in our environment a greater impact in patients and their parents lifes. It appears to be important to stablish a scheduled analgesic treatment for the first 10 days after surgery.
KEYWORDS: pain; children; tonsillectomy; Wong Baker scale
RESUMEN: Introducción y objetivo: El dolor en niños ha sido siempre un reto terapéutico. La amigdalectomía es una cirugía muy prevalente y dolorosa, la cual aun presenta barreras para garantizar un adecuado control analgésico. El objetivo fue describir la mediana de dolor postoperatorio en niños entre 3 y 8 años que han sido intervenidos de una cirugía amigdalar. Método: Se realizó un estudio descriptivo, observacional, prospectivo y longitudinal en niños de 3 a 8 años del Hospital Universitario Quirón Pozuelo Madrid intervenidos de amigdalectomía durante el año 2020. La recogida de datos se realizó mediante un cuestionario de dolor, marcando la intensidad de este del 0-10 en la escala de dolor de Wong Baker (basado en dibujos con caras). Además, completaron otras preguntas sobre la indicación quirúrgica, los días lectivos perdidos por el niño y los laborables por los padres y la analgesia que recibió el niño. Resultados: Se incluyeron 29 pacientes, 14 niñas y 15 niños con una mediana de edad de 4. La mediana de dolor más alto se encontró el 2º día con un valor de 3,0. Por tanto, elegimos el 2º día para comparar la magnitud de dolor entre las distintas indicaciones. En función de la indicación quirúrgica, la mediana de dolor por obstrucción fue de 3,0, en cambio fue de 4,0 en los intervenidos por obstrucción en conjunto con alteraciones del crecimiento facial. Los niños perdieron una mediana de 8 días en el colegio y los padres perdieron una mediana de 2 días cada uno en el trabajo. Discusión: Los datos límitados que tenemos sugieren que la cronicidad de la obstrucción por la hipertrofia amigdalar dando lugar a alteraciones del crecimiento facial hizo la operación más dolorosa y además, el dolor tuvo unas mayores consecuencias en la vida diaria del paciente y sus progenitores. Es de gran importancia esforzarnos en cumplir una pauta analgésica en el postoperatorio los 10 primeros días.
PALABRAS CLAVE: dolor; niños; amigdalectomía; Wong Baker
INTRODUCTION
Tonsillectomy is one of the most common surgical procedures performed in children, and among the most painful ones [1]. Surgery consists in the extirpation of the palatine tonsils, which are nodes of lymphoid tissue associated with the mucosa and are part of the Waldeyer´s ring located in the pharynx [2]. The most frequent indications for the extirpation of the tonsils are the obstruction of the upper airway and recurrent infections. The obstruction is caused by the hypertrophy of the tonsils, most commonly due to repetitive infections that make the tonsils grow [3]. This can make children suffer from obstructive sleep apnea (OSA), a condition where the patient stops breathing for a period of time in a high number of occasions through the night. If the child also suffers from obesity or facial growth problems the probability of suffering from OSA increases exponentially [4]. The prevalence OAS in children is about 2-5 %. Studies have found that children with OAS have 4,11 more risk of suffering from a left ventricular hypertrophy. Children with severe OSA have an increased risk of nearly 14 times of suffering sudden death or heart failure [5]. Another prevalent complication is behavioral and cognitive problems such as attention deficit - hyperactivity disorder (ADHD). A cohort study found that in children who were on a waiting list for tonsil surgery around 30 % suffered ADHD [6].
Tonsillectomy is highly effective. A study showed that 80 % of the children with OSA improved with tonsillectomy (as proved by polysomnography) and they experienced greater life quality and had a decrease in behavioral and cognitive problems [7]. However, it is considered a surgery with a high rate of complications. Up to almost 10 % of the patients may suffer primary or secondary bleeding [8]. Around 7-13 % of the children who underwent a tonsil surgery came back to emergency, 15 % because of uncontrolled pain and 25 % due to nausea, vomits and dehydration, partly also related to pain [9]. Therefore, pain is an important factor for comorbidity and complications around surgery.
Pain is the subjective feeling of the tissues being injured [10]. In order to measure this feeling in kids we use graphic pain scales. In kids between the age of 3 to 8 years we measure the pain with an autodiagnosis tool called the Wong-Baker scale. This is a scale that shows the kids a number of drawn faces expressing different feelings. If there is no pain (0) it is associated with a smiley face. This face gets sadder and sadder until it cries, which means the maximum pain intensity [11] (Figure 1).
Figure 1. Questionnaire based on the Wong Baker pain scale to measure pain during follow up. Children had to mark the faces with the help of their parents. Additional questions had to be answered by the parents.

These scales based on drawings have proved to be really useful in the day-by-day clinic. Also, children understand it independently of the geographic or cultural situation [12].
However, we face a therapeutic challenge due to the myths around pain in children. People are prone to think that children experience less pain. There is a lot of misunderstanding about opioids and its side effects in children [13]. In outpatient surgery, where pain control escapes from the hospital environment, we find ourselves in a greater difficulty. It has been shown that only 35 % of the parents gave their children the analgesia that was prescribed by the doctor. Parents declared that they did not give the pain killers because they feared the side effects or that they will create an addiction. They also declared that pills should be used as a last resource [14]. It is also thought that the greater the exposure to pain the greater the tolerance to it: it has been shown that the effect is the complete opposite, causing a hypersensibilization to pain [15].
Therefore, the more we know on pain associated with tonsillectomy in children, the better we are fitted to approach it. We could also teach the parents the importance of a better pain control. And finally, we could get less comorbidities, a faster rehabilitation and reduce suffering both for children and their parents.
The aim of this study is to make a quantitative description of pain after tonsil surgery in children between 3 and 8 years.
MATERIAL AND METHODS
We designed a descriptive, observational and prospective study on patients between 3-8 years old who underwent a tonsillectomy at a university hospital between November 2019 and March 2020. We excluded children that had a hospital admission in the last year, those who had a chromosomic disease or an immune disorder. Also, patients who did not fulfill the whole of the questionnaire were excluded.
All of the procedures were performed by the same surgeon (JHC). Tonsillectomy was performed with a radio-frequency device (Coblator® 2).
Smith and Nephew) and the standard analgesic prescription was to alternate acetaminophen (15mg/kg) and metamizole (40mg/kg) every 4 hours. They could also use deflazacort (1mg/kg) the 3rd and 4th days after the procedure as a rescue treatment if pain was not well controlled.
We gave the parents a questionnaire the day of the surgery which they had to fulfill with their children. Children had to choose in the Wong-Baker scale according to how they felt. They fulfilled the questionnaire every day for 2 weeks and they handed out the questionnaire at the follow-up visit the next month.
We also asked about the days that the kid lost at the school and the days that the parents lost at their work. Also, if they had to take acetaminophen, metamizole (Metalgial®) or corticoids (Zamene®). The questionnaire was handed out along with the informed consent and the information brochure with the purpose of the study well explained. They freely decided if they wanted to be included in the study. Further data were included: age, gender, the indication for surgery (upper airway obstruction, chronic infection, facial growth disorders).
For the qualitative variables we calculated the absolute and relative percentages. For the quantitative variables we calculated the mean and the standard deviations in the case that the distribution was normal (according to the Kolmogorov-Smirnov test) and the median and the interquartile range if it was not.
The protocol was accepted by the ethic committee.
RESULTS
We collected the information from 30 patients. Fourteen were girls (48.28 %) and 15 boys (51.72 %). They had an age between 3 and 8 years old according to inclusion criteria. The median age of the patients that underwent surgery was 4.0 (p25-p75=3.0-6.0). There were no statistical differences according to gender and most of the patients were between 3 and 5 years old (72.41 %). The most frequent indication for surgery was obstruction (65,52 %), followed by obstruction plus chronic infection and obstruction plus facial growth disorders, with a percentage of 13,79 % and 10,34 % respectively (Figure 2).
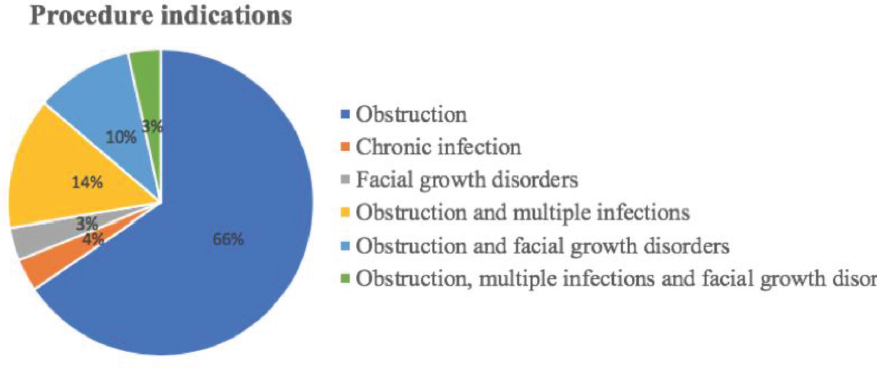
Figure 2. Procedure indications. Percentage of the different procedure indications.
Pain was measured from 0 to 10 following the Wong Baker pain scale for 15 days. Median values and the p25-p75 are showed in table 1. The highest value was found the second day after surgery with a median of 3,0 (p25-p75=2,0-6,0). After the 10th day median values were 0,0.
Table 1. Pain from 0-10 the first 15 days.
Pain 0-10 |
Median (p50) |
p25-p75 |
Day 1 |
2,0 |
0,0-4,0 |
Day 2 |
3,0 |
2,0-6,0 |
Day 3 |
2,0 |
0,0-4,0 |
Day 4 |
2,0 |
0,0-5,5 |
Day 5 |
2,0 |
0,0-4,0 |
Day 6 |
2,0 |
0,0-6,0 |
Day 7 |
2,0 |
0,0-6,0 |
Day 8 |
2,0 |
0,0-6,0 |
Day 9 |
2,0 |
0,0-4,0 |
Day 10 |
2,0 |
0,0-3,5 |
Day 11 |
0,0 |
0,0-2,0 |
Day 12 |
0,0 |
0,0-0,0 |
Day 13 |
0,0 |
0,0-0,0 |
Day 14 |
0,0 |
0,0-0,0 |
Day 15 |
0,0 |
0,0-0,0 |
Acetaminophen was the most used pain-killer with a median of intake of 7 tablets (p25-p75=2,0-15,25) during the 15 days. The median intake of metamizole was 2 tablets (p25-p75=0-2) during the 15 days, and the percentage of the patients that needed to take corticotherapy was 22,22 %.
Children lost a median of 8 days (p25-p75=7,0-10,0) at school and the days lost at work by their fathers and mothers had a median of 2 (p25-p75=0,0-5,0) and 2 (p25-p75=1,0-3,0) respectively. There were no statistically significant differences between the mother and the father. If we consider the values of the patient that suffered the most pain (6,4) we can observe that the days lost at school were 21 days and that both parents had to lose 14 days at work. For the patient with least pain (0) the child only lost 1 day at school and their parents did not have to absent any day from work.
If we describe the median pain value during the first 15 days, we can see that the second day was the day with the most pain. If we take this value as a representative value and we compare it between both genders we find that girls tended to have more pain than boys with a median of 4,0 (p25-p75=2,0-6,0) in comparison with boys that had a median of 2,0 (p25-p75=2,0-6,5). If we compare this same value with the age of the children, we find that the median with more pain are children 4 years old, with a median of pain of 4,0 (p25-p75=2,0-6,5).
If we take again the median of the second day of pain and we compare it with the indication for surgery we find that surgery indication that resulted with less pain was for patients that underwent surgery because of airway obstruction (with a value of 3,0; p25-p75=2,0-6,0). On the other hand, we found that children with obstruction plus facial growth disorders had more pain, with a median of 4,0 (p25-p75=2,0-6,0). We found similar days lost between the mother and the father, with a median of 2,0 (p25-p75=0,0-5,0) and 2,0 (p25-p75=1,0-3,0) respectively (Table 2).
Table 2. Days lost at the school by the children and at work by the parents.
Days lost |
|
|
|
Median |
p25-p75 |
Kids at school |
8,0 |
7,0-10,0 |
Mother at work |
2,0 |
0,0-5,0 |
Father at work |
2,0 |
1,0-3,0 |
DISCUSSION
The most usual indications for tonsillectomy in children that we found were airway obstruction and recurrent tonsillitis.
We found that children with airway obstruction and facial growth disorders experienced more pain. Obviously early diagnosis and treatment would prevent the growth disorder itself but as a side effect it might also avoid tonsillectomy related morbidity.
We found a direct relationship between the pain that the children suffered, and the impact surgery had in their life`s. The higher the pain, the more lost days at school and the more impact in the laboral life of their parents. If we translate the days lost, at economic loss and considering that the average wage in Spain in 2017 was 25417,75 euros a year [16] and we add up the total of days lost from both parents for the child with the highest pain, it would amount a loss of 2695,72 euros. Conversely for the kid with less pain, he only lost 1 day of school (the day of the surgery) and neither parent lost any day at work. We have to point out that the study was held in a hospital located in a high socioeconomic level environment which could influence some of the variables.
Taking in count that the median of intake for the acetaminophen was 7 tablets (p25-p75=2,0-15,25) and that the median intake of metamizole was 2 tablets (p25-p75=0-2) during the 15 days and knowing that children can take a maximum of 3 tablets per day for both pills, we conclude the following conclusion. The maximum days that they took as an average were only 2 and a half days (following the median of tablets taken), and most of them didn´t alternate with the metamizole. So, this reflects most of the parents did not give the analgesic treatment as prescripted and neither the sufficient days to have a good pain control.
A limitation of the study was that the pain of the child could be biased if the kid was given or not analgesic treatment. We might try to instruct parents on the benefits of adequate pain management, but we have to count with this fact.
But one of the strengths of the study is that we can point out is that we could watch day by day the behavior of the pain and identify the most critical phases, and in addition, analyze it with more detail. Also, we collected the data prospectively, avoiding memory or information bias.
CONCLUSIONS
Safe analgesic medication is available to treat postoperative pain in children after tonsillectomy. Is seems rational to establish a treatment guideline for the first 10 days after the surgery which adapts medication to the level of pain and have a prescripted treatment for the first 2-3 days, which are the ones with the most pain. Also, to step up and give the prescripted treatment longer for children when they show ogival palate in addition to airway obstruction which had shown a higher pain. In addition, we have to tell and give information to the parents about the safety of the analgesic treatment and the importance on a good control of the pain, which is the principal comorbidity of the procedure and to avoid suffering to the children before the pain arises.
Although it is an already extensively studied field. There appears to be areas to investigate more around the pain in children after tonsillectomy. The aim is to reduce the morbidity and the direct consequences in daily life caused by a inadequate handling of pain.
REFERENCES
1.Vons KMJ, Bijker JB, Verwijs EW, Majoor MHJM, De Graaff JC. Postoperative pain during the first week after adenoidectomy and guillotine adenotonsillectomy in children. Paediatr Anaesth. 2014;24(5):476–82.
2.Macaya Martínez A, Arruti González I, Quer Canut S. Amigdalectomía y adenoidectomía. Indicaciones, técnicas y complicaciones. Libr virtual Form en ORL. 2014;1–15.
3.Gozal D, Tan H-L, Kheirandish-Gozal L. Obstructive sleep apnea in children: a critical update. Nat Sci Sleep. 2013 Sep;109.
4.Mechanisms and predisposing factors for sleep-related breathing disorders in children - UpToDate [Internet]. [cited 2020 Feb 23]. Available from: https://www-uptodate-com.ezproxy.universidadeuropea.es/contents/mechanisms-and-predisposing-factors-for-sleep-related-breathing-disorders-in-children?sectionName=Enlargedtonsilsandadenoids&search=osachildren&topicRef=6363&anchor=H12&source=see_link#H12
5.Hanlon CE, Binka E, Garofano JS, Sterni LM, Brady TM. The association of obstructive sleep apnea and left ventricular hypertrophy in obese and overweight children with history of elevated blood pressure. J Clin Hypertens [Internet]. 2019 Jul 1 [cited 2020 Feb 23];21(7):984–90. Available from: https://www.ncbi.nlm.nih.gov/pubmed/31222948
6.Cognitive and behavioral consequences of sleep disorders in children - UpToDate [Internet]. [cited 2020 Feb 23]. Available from: https://www-uptodate-com.ezproxy.universidadeuropea.es/contents/cognitive-and-behavioral-consequences-of-sleep-disorders-in-children?sectionName=Sleep-relatedbreathingdisorders&search=osachildren&topicRef=6373&anchor=H16053990&source=see_link#H16053990
7.Adenotonsillectomy for obstructive sleep apnea in children - UpToDate [Internet]. [cited 2020 Feb 23]. Available from: https://www-uptodate-com.ezproxy.universidadeuropea.es/contents/adenotonsillectomy-for-obstructive-sleep-apnea-in-children?search=osachildren&source=search_result&selectedTitle=4~150&usage_type=default&display_rank=4
8.De Luca Canto G, Pachêco-Pereira C, Aydinoz S, Bhattacharjee R, Tan H-L, Kheirandish-Gozal L, et al. Adenotonsillectomy Complications: A Meta-analysis. Pediatrics [Internet]. 2015 Oct 1 [cited 2020 Feb 23];136(4):702–18. Available from: https://www.ncbi.nlm.nih.gov/pubmed/26391937
9.Tonsillectomy (with or without adenoidectomy) in children: Postoperative care and complications - UpToDate [Internet]. [cited 2020 Feb 23]. Available from: https://www-uptodate-com.ezproxy.universidadeuropea.es/contents/tonsillectomy-with-or-without-adenoidectomy-in-children-postoperative-care-and-complications?sectionName=COMPLICATIONS&search=osachildren&topicRef=97855&anchor=H7658117&source=see_link#H7658117
10.Longo D, Fauci A, Kasper D, Hauser S, Jameson L, Loscalzo J. Harrison: principios de medicina interna (18° ed). In: Harrison Principios de Medicina interna. 2012.
11.Evaluation and management of pain in children - UpToDate [Internet]. [cited 2019 Oct 22]. Available from: https://www-uptodate-com.ezproxy.universidadeuropea.es/contents/evaluation-and-management-of-pain-in-children?search=approachto evaluation of pain in children&source=search_result&selectedTitle=9~150&usage_type=default&display_rank=9#H3
12.Young JR, Sih C, Hogg MM, Anderson-Montoya BL, Fasano HT. Qualitative Assessment of Face Validity and Cross-Cultural Acceptability of the Faces Pain Scale: «Revised» in Cameroon. Qual Health Res [Internet]. 2018 Apr 1 [cited 2020 Feb 23];28(5):832–43. Available from: https://www.ncbi.nlm.nih.gov/pubmed/29571279
13.Bawa M, Mahajan JK, Aggerwal N, Sundaram J, Rao KLN. Barriers to Pediatric Pain Management in Children Undergoing Surgery: A Survey of Health Care Providers. J Pain Palliat Care Pharmacother [Internet]. 2015 Oct 2 [cited 2020 Feb 23];29(4):353–8. Available from: https://www.ncbi.nlm.nih.gov/pubmed/26654407
14.Dorkham MC, Chalkiadis GA, Von Ungern Sternberg BS, Davidson AJ. Effective postoperative pain management in children after ambulatory surgery, with a focus on tonsillectomy: Barriers and possible solutions. Vol. 24, Paediatric Anaesthesia. 2014. p. 239–48.
15.Brasher C, Gafsous B, Dugue S, Thiollier A, Kinderf J, Nivoche Y, et al. Postoperative pain management in children and infants: An update. Pediatr Drugs. 2014;16(2):129–40.
16.Salario anual medio, mediano, modal, a tiempo completo y a tiempo parcial, por periodo.(10882) [Internet]. [cited 2020 Mar 29]. Available from: https://www.ine.es/jaxiT3/Datos.htm?t=10882#!tabs-tabla