ISSN electrónico: 1885-5210
DOI: https://doi.org/10.14201/rmc.32031
THE SERPENT AND THE RAINBOW (1988): A PATHOPHYSIOLOGICAL MODEL FOR TETRODOTOXIN OVERDOSE
La Serpiente y el Arco Iris (1988): un modelo fisiopatológico por sobredosis de tetrodotoxina
Carmen FERNÁNDEZ-MARTOS1, Nora SULEIMAN-MARTOS2, José Luis GÓMEZ-URQUIZA3, Isabel PRIETO-GÓMEZ4, Manuel RAMÍREZ-SÁNCHEZ4, Ana Belén SEGARRA-ROBLES4, Francisco GARCÍA-CÓZAR5, Germán DOMÍNGUEZ-VÍAS6
1Department of Pharmacology, CEU San Pablo University, Madrid (Spain).
2Department of Nursing, Faculty of Health Sciences of Granada. University of Granada (Spain).
3Department of Nursing, Faculty of Health Sciences of Ceuta. University of Granada (Spain).
4Physiology Area, Faculty of Experimental Sciences. University of Jaén (Spain).
5Immunology Area, Faculty of Medicine. University of Cádiz (Spain).
6Department of Physiology, Faculty of Health Sciences of Ceuta. University of Granada (Spain).
Corresponding Author: Germán Domínguez-Vías
Email: germandv@ugr.es
Received: 29 de marzo de 2024
Accepted: 26 de junio de 2024
Abstract
The Serpent and the Rainbow (1988) is an attractive teaching model that combines pharmacology and physiological alterations in many functional systems. Based on a true event, this horror classic turned into a cult film analyzes how the scientific method is capable of providing answers to the myth of the living dead through voodoo, in the population of Haiti, due to the inhalation of a powerful powder drug that contains high doses of tetrodotoxin. This film simulates the acute state of catalepsy of the patients and the tests submitted to certify the apparent death after confirmation of the irreversible cessation of cardiorespiratory or brain functions, due to the absence of brainstem reflexes from the long-term effects of the drug. Furthermore, although the patient does not die and is buried while being aware of the entire process, the film allows the students to reflect on the high psychological burden, both of the patient himself and of the population, which deepens the states of terror by assuming who is a slave returned from death without soul and without will.
Keywords: physiology; homeostasis; tetrodotoxin; TTX; neurotoxin; voodoo.
Resumen
La Serpiente y el Arco Iris (1988) supone un modelo docente atractivo que combina la farmacología y las alteraciones fisiológicas en muchos sistemas funcionales. Basada en un hecho real, este clásico del terror convertida en una película de culto analiza como el método científico es capaz de dar respuestas al mito del muerto viviente, a través del vudú en la población de Haití, por la inhalación de una potente droga en polvo que contiene altas dosis de tetrodotoxina. Este filme simula el estado agudo de catalepsia de los pacientes y las pruebas sometidas para certificar la aparente defunción tras la confirmación del cese irreversible de las funciones cardiorrespiratorias o encefálica, debido a la ausencia de reflejos troncoencefálicos a causa de los efectos a largo plazo que presenta la droga. Además, a pesar de que el paciente no fallece y es enterrado siendo consciente de todo el proceso, el filme permite reflexionar en los estudiantes la alta carga psicológica, tanto del propio paciente como de la población, que profundiza en los estados de terror al suponer que es un esclavo retornado de la muerte sin alma y sin voluntad.
Palabras clave: fisiología; homeostasis; tetrodotoxina; TTX; neurotoxina; vudú.
Technical details
Original title: The Serpent and the Rainbow.
Other Titles: La Serpiente y el Arco Iris.
Country: United States.
Year: 1988.
Director: Wes Craven.
Screenwriter: Richard Maxwell, Adam Rodman, Wade Davis
Music: Brad Fiedel.
Photography: John Lindley.
Film editor: Glenn Farr.
Cast: Bill Pullman, Cathy Tyson, Zakes Mokae, Paul Winfield, Brent Jennings, Conrad Roberts, Badja Djola, Theresa Merritt, Michael Gough, Paul Guilfoyle, Dey Young, Aleta Mitchell, William Newman.
Color: Color.
Duration: 98 min.
Genre: Fancy. Terror. Cult film.
Original language: English.
Production Company: Universal Pictures.
Synopsis: A Harvard anthropologist is sent to Haiti to investigate a strange substance related to black magic and voodoo, which could be used to save human lives. While he searches for the miraculous drug, certain skeptical scientists refuse to accept the existence of zombies and bloody rites. (FilmAfinity).
Awards: Nominee 1990, Saturn Awards: Best Make-Up (David LeRoy Anderson, Lance Anderson).
Availability: The Serpent & The Rainbow [Blu-ray]. Company: Reel One Films.
Links:
Tráiler Internacional (VO):
https://www.filmaffinity.com/es/evideos.php?movie_id=705831
https://www.imdb.com/video/vi3782412057/?playlistId=tt0096071&ref_=tt_pr_ov_vi

Original poster
Introduction
The beginning of The Serpent and the Rainbow (1988) narrates that “In the legends of the Serpent is a symbol of Earth. The Rainbow is a symbol of Heaven. Between the two, all creatures must live and die. But because he has a soul, man can be trapped in a terrible place where death is only the beginning”. This beginning is not much different from the beginning of any physiologically based book, where it is explained that homeostasis predominates in the human body, that is, the state of balance between all the body systems necessary to survive and function properly. This film reflects how psychoactive drugs are capable of breaking this homeostasis to the limits of pathophysiology.
The film is partially based on a book of the same name written in 1985 by the Canadian anthropologist, ethnobotanist, writer and photographer Wade Davis1 where he refers to his experiences in Haiti. There he investigated the story of Clairvius Narcisse, a man allegedly poisoned, buried alive, and victim of a process of zombification. The film takes place with the figure of Dr. Dennis Alan of Harvard (Bill Pulman) who brings to life the true story of Wade Davis. This story tells how the scientist travels to Haiti in the first decade of the 80s to look for the recipe for a drug, which resembles a yellow powder, with the pretext of applying it in clinical research. The recipe for this powder, known in their language as coup de poudre, once inhaled, strips away the sanity and will to enslave the affected person and turn them into a living dead, which in modern times is also known as a zombie. This occurs at a critical moment in Haiti’s history, during the government of dictator Jean-Claude Duvalier.
A first scene from Haiti in 1978 shows how different medical tests are performed that allow us to discriminate between real death and apparent death. Medical action through rudimentary tests of the time, such as cardiorespiratory tests and nervous reflexes, allow us to certify the death of a Haitian patient named Christophe Durand who dies mysteriously in a French missionary clinic while a voodoo parade passes in front of his window. The absences of physiological responses are many and varied: pulse, heartbeat (Photo 1A), mist exhaled on the stethoscope (Photo 1,B-C), doll’s eye reflex, ocular nervous stimulation due to pupil dilation, as well as brain impulses and pain stimuli (Photo 1, D-E). The lack of evaluation of sensory, motor and pain stimuli determines a report of death due to cardiorespiratory arrest and cerebral death (also known as brain death) (Photo 2, A-D).
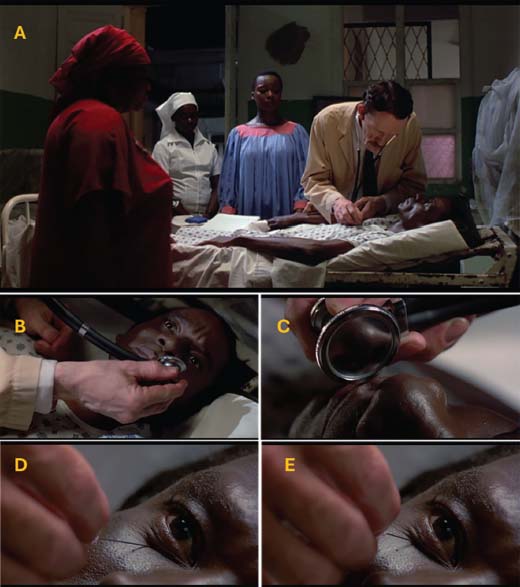
Photo 1. Auscultation test (A) and respiratory exhalation test (B-C), showing absence of signs of cardiorespiratory death. Pain stimulus test by puncturing the margin of the inferior orbicularis muscle (orbital portion of the right eye), showing absence of nervous reflexes as no grimaces or facial movements appear, suggesting a diagnosis of brain death (D-E)
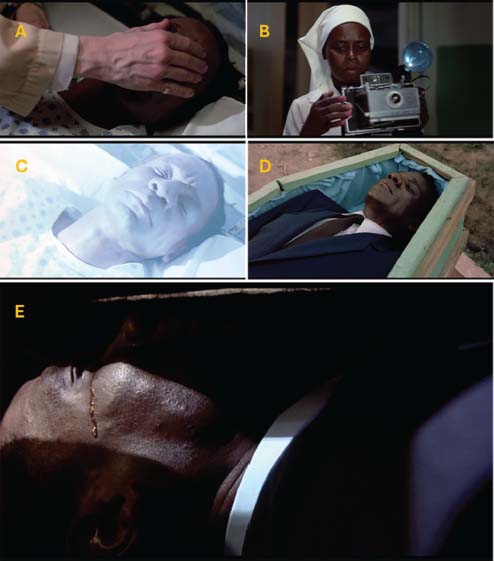
Photo 2. Photographic taking for the death certificate (A-C) and burial (D). Apparent death, Durand cries and shows awareness of what happened (E)
However, during the burial it is observed inside the coffin that the deceased cries while manifesting an acute process of catalepsy (Photo 2E). Seven years later he is seen alive again (Photo 3).

Photo 3. Medical death certificate (right) and recent document proving that he is alive seven years later (left)
In 1985, after successful research in the Amazon rainforest with a local shaman studying samples of medicinal plants and unknown hallucination-inducing drugs, Dr. Alan is invited as an advisor by the president of the pharmaceutical industry BIOCORP of Boston, Andrew Cassedy. Dr. Alan is tasked with traveling to Haiti to investigate the case of a native man named Christophe Durand. Durand died in 1978 and apparently came back to life. The president of the pharmaceutical industry is interested in learning about the zombification drug. Cassedy shows the death and burial certificate at the same time that he shows a photograph that shows that Durand is still alive (Photo 3). The meeting explains the need to obtain samples of this voodoo drug and replicate the results of the resurrected Durand, with the intention of producing a powerful anesthetic drug that will revolutionize medicine by helping to save deaths in operating rooms. Dr. Alan arrives in Haiti at the start of a revolution to meet Dr. Marielle Duchamp, who is treating zombified patients like Margrite and Durand. Dr. Alan asks Durand what he remembers when he died and he answers that he remembers everything, from how they threw dirt on his coffin and the sorcerer taking his soul, depriving him of his freedom by appearing in people’s dreams. Durand explains that it is a poisonous dust that enters through the skin until it reaches the soul.
Soon Dr. Alan is threatened by the head of the dictator’s secret police and personal militia, leader of the Tonton Macoutes (bogeymen in English), Dargent Peytraud, who is a torturer and a powerful witch. Dr. Alan has nightmares of Peytraud, who is revealed to be a bokor (sorcerer) who turns enemies into zombie slaves and steals their souls.
Later, Dr. Alan contacts Louis Mozart, a Haitian with knowledge to carry out the chemical synthesis and purification of the powdered zombie drug. The drug has four identified ingredients: 1) poisonous sea toad (Bufo marine, Rhinella marina) scared with a stinger of a sea worm (possibly the fireworm or Hermodice carunculata) to produce more venom; 2) local poisonous tetrodotoxin (TTX)-producing fish (Fugu-like puffer fish); 3) Mixture of herbs and minerals; 4) pulverized bones from the skull of a corpse. The process of making the drug lasts three days and three nights. The powder, once prepared, must follow the maturation ritual by burying it for another day with the corpse (Photo 4). The powder cannot be ingested with food, and can kill instantly.

Photo 4. Ingredients to create the zombification voodoo powder: (A) poisonous toad, (B) fish rich in tetrodotoxin, (C) mixture of herbs and minerals, (D) ground corpse cranial bone. (E) Final result of voodoo powder
Analysis of the powder in the laboratory shows that it is a powerful anesthetic, which can be jokingly called Zombanol. It is described that the drug was tested on baboons by putting powder on their hands. The dust was able to pass through the skin and reach the blood, and 10 – 20 minutes later they seemed more dead. The results showed important significant changes (Photo 5).

Photo 5. Empirical results carried out on baboons after the administration of voodoo powder. (A) The acute drug reaction causes a clear association of the loss of vital signs (pulse, blood pressure and tidal volume along with respiratory rates) with changes in activity in the hemispheres. (B) Despite the apparent death, they show a sign of consciousness when studying the electroencephalographic recording, detecting different recordings of the amplitude of the wave at different times in different nervous systems, such as the limbic, sensory, autonomic and motor systems
The animals’ brain scans were very limited and only acted on certain parts of the brain. The values of vital functions, breathing and heart rate seem as if they have been disconnected with a switch (Photo 5A), but the parts of the brain that control sensations, thoughts and emotions allow us to know what is constantly happening to them (Photo 5B). The same thing happens in a human, they can see, feel and think, but they cannot act in any way, remaining inert. In Haiti, the victims remain cataleptic, watching the entire process, buried alive. The effects of the dust revert after twelve hours, recovering normal physiological functions, only then he will be under two meters of earth, in the dark and without air, scratching and screaming without anyone hearing him suffocate.
The end of the film explains that “the zombie powder and its active ingredient, tetrodotoxin, is currently under intensive scientific study both in Europe and the United States. To this date the process by which it works remains a mystery”.
Results and Discussion
Catalepsy or apparent death
Catalepsy is a biological state in which the person lies motionless, in apparent death without vital signs; however, they are in a conscious state that can vary due to reflex actions. Although the symptoms of catalepsy are similar to that of apparent death, the recordings of the electrical signal of the heart with an electrocardiogram (ECG) will be the definitive proof that will allow death to be certified. In the film he confirms that the physician’s expertise fails due to the absence of an electrocardiography during the acute episode of catalepsy. The state of apparent death induced by the voodoo drug drastically reduces breathing, reflex stimuli, blood pressure and pulse with rates so low that they are confused with clinical death. Drugged patients show syncope due to a clear clinical case of orthostatic hypotension2, which is defined as a drop of ≥20 mmHg in systolic blood pressure and/or ≥10 mmHg in diastolic blood pressure within 3 minutes of active standing. After tilt-induced syncope, blood pressure generally recovers rapidly after returning to the horizontal position3, 4. However, in some patients, hemodynamic recovery is delayed, a condition recently termed “prolonged postfainting hypotension”. The mechanism is believed to be mediated by a delay in the recovery of cardiac output as a consequence of increased vagal flow4, rather than exaggerated peripheral vasodilation and sympathetic withdrawal. Durand’s survival in the face of prolonged hypotension is because he was in a horizontal position, allowing blood to be easily pumped in the same plane.
Complementation with recordings of the brain’s electrical activity by electroencephalogram (EEG) would have helped reduce these errors. A clinical study with animals demonstrates that catalepsy induced by another drug, morphine, consists of two complementary5, but opposite extreme behaviors (rigid immobility and sudden locomotor bursts), each of which can be controlled by different kinds of external stimuli. Phasic (discrete) stimulation produces behavioral and/or EEG activation, however, in a very similar way to the resurrected Durand, when the stimuli involving pain and/or nociceptive skin pressure are tonic (continuous), the EEG deactivation induced by morphine and behavioral immobility, even to the point of stimulation-linked reversible coma. Furthermore, this apparent death of the character due to the drug is also similar to that of animals that become immobilized before a predator. The sensorimotor characteristics and EEG reactions suggest that there may be similarities between morphine-induced catalepsy and the defensive reactions of immobility and escape in drug-free animals (i.e., the adaptive reflex of feigning death)5.
The medical death certificate
Long before the appearance of recordings of bioelectric signals, until a few decades ago, the limits of life and death were determined by the existence or not of cardiac and respiratory activity. The concept of death was expanded when it was discovered that the brain had a vital role in governing physiological functions, therefore, the reversible cessation of the functions of the central nervous system (CNS) must also be considered death6. Although the definition of clinical death is apparently obvious, it is more complex than it seems. The need to unify criteria led to the establishment in the United States (USA, 1981)7, 8 of two possibilities for diagnosis (President´s Commission): 1) Irreversible absence of cardiovascular and respiratory functions, or 2) Irreversible cessation of all brain functions (brain and brainstem). Since the brain is the organ that coordinates the physiology of the entire organism, when brain death occurs, profound pathophysiological changes appear that lead to the deterioration and subsequent cessation of the functions of the different organs and systems. These changes are associated with alterations6, 9, 10: 1) hemodynamics with a previous parasympathetic appearance and explosive sympathetic response; 2) respiratory due to the presence of apnea; 3) thermoregulation due to destruction of the thermoregulatory centers of the hypothalamus with frequent occurrence of hypothermia; 4) endocrine metabolic with the appearance of diabetes insipidus, loss of electrolytes in urine, hyperglycemia due to the release of catecholamines and low demand for cellular metabolism. In some patients who meet the criteria for brain death, spinal reflexes may falsely suggest persistence of brain function8, 9.
For clinical neurological examination, it is necessary to perform different tests in an orderly manner to avoid interference in the results. To certify brain death it is necessary to identify10:
A. Absence of brain functions:
When brain death is diagnosed, the person has no reflexes and is also in apnea. There is nonreactive coma without any type of motor or vegetative response to the intense pain stimulus at the supraorbital level (cranial nerve territory). It is not assessable in the presence of deep sedation or neuromuscular blocking agents. However, on some occasions, there are brain-dead people who have spontaneous muscle contractions. Spontaneous or induced motor activity of spinal origin does not invalidate the diagnosis of brain death. Regarding the latter, the most frequent reflexes are the cutaneous-abdominal, cremasteric, plantar flexor, withdrawal reflex and tonic-cervical (cervical-flexor of the arm, hip or cervico-abdominal). Flexion of the trunk and tonic contractions of the upper limbs may also appear, known as the “Lazarus sign”.
B. Absence of brainstem activity due to:
a) Atropine test, to explore the destruction of the nucleus ambiguus, or; b) Abolition of type reflexes: 1) photomotor, applying a light stimulus to both eyes and without producing pupillary contraction (unless under the effect of anticholinergic eye drops or with atropine in the blood); 2) corneal, stimulating both corneas with a gauze or cotton swab does not produce eyelid contraction or tearing (unless under the effect of neuromuscular blocking drugs as is the case with the film); 3) oculocephalic or “doll’s eyes” reflex, keeping the patient’s eyes open and causing rapid turns of the head in a horizontal (or vertical) direction, the combined deviation of the gaze in the opposite direction to the turn of the head does not occur, always staying in your initial position with a fixed gaze; 4) oculovestibular, the patient’s head is kept elevated 30° above the horizontal with both eyes open. 50 mL of cold serum is injected through a probe through the external auditory canal. Brain death is confirmed if in one minute there is no response of nystagmus with deviation of the eyes to the irrigated ear and another rapid one that takes them away from the sensation of cold (unless there is pharmacological toxicity due to sedatives or antiepileptics as occurs in the film).
While the EEG reflects spontaneous brain bioelectric activity, evoked potentials represent the CNS response to a specific external stimulus. Theoretically, any stimulus capable of producing depolarization of a peripheral nerve (sensory or mixed) can be used to provoke evoked responses at the CNS level. Currently, only visual, acoustic and someesthetic evoked potentials are used in routine clinical practice because they are resistant to central depressants and hypothermia and provide useful information to diagnose brain death11.
Tetrodotoxin as an ingredient in voodoo powder
In this way, the zombie of Haitian society is a living dead achieved with ethnopharmacological preparations. The poisonings that arise from the therapeutic activities belonging to the voodoo cult are similar to that of the drug of modern medicine. Although Haitian voodoo priests control herbal healing, for the practice of poisoning poisons are extracted from tissues (plant and animal) and then administered to victims as a means of punishment established by a clandestine justice system12. The zombie drug used as a powder acts as a dissociative anesthetic agent, possessing primary psychoactive hallucinogenic and neurotoxic effects with plasma clearance that may take hours to weeks. Of the four ingredients identified in the film, the analgesic and anesthetic effects of the drug come from the sea toad and the TTX-producing fish, especially the latter. In non-fiction, the formula of the poison is known in four widely separated localities in Haiti, including as an ingredient one or more species of puffer fish (Diodon hystrix, Diodon holacanthus or Sphoeroides testudineus) that contain lethal amounts of the neurotoxin TTX, capable of pharmacologically induce the zombie state13. Pufferfish contain TTX in the organs, especially the region of the liver and ovaries, and also in the skin. TTX binds to voltage-gated sodium channels of human muscles and excitable nervous tissues, blocking it and thereby inhibiting the entry of sodium ions and arresting impulse conduction by impairing action potential propagation, resulting in hypotension (more due to peripheral vasodilation than depression of cardiac activity), numbness, nervous paralysis of the diaphragmatic muscles and immobilization14. The venom paralyzes the muscles while the victim remains fully conscious and eventually dies from respiratory paralysis (asphyxiation), accompanied by paresthesia, headache, blurred vision, vertigo, nausea, vomiting and hypothermia15, 16. Intoxication is easily detectable by a TTX-specific enzyme-linked immunoassay (ELISA) in blood and urine17.
There is currently no known antidote, and the standard medical approach is supportive treatment to attempt to support the respiratory (assisted ventilation) and circulatory (hemodialysis) systems until the poison is eliminated15, 16. Chances of survival improve with gastric lavage and/or oral ingestion of activated charcoal, intravenous hydration, and neostigmine injections to increase activity at the neuromuscular junction18. Neostigmine, a parasympathomimetic that acts as a reversible inhibitor of the enzyme cholinesterase19, continues to be investigated as a possible treatment.
Food poisoning due to pufferfish is very common, where prevention is born with the implementation of measures to increase awareness, control markets and establish toxicological tests17. In 2008, advances in fugu research and cultivation have allowed some fish farmers to massively produce non-toxic specimens. The researchers found that the TTX in fugu came from eating other animals that had TTX-producing bacteria20, and they developed immunity over time.
More research agrees that this powder contains an alkaline degradation product of TTX12, 21, achieved through extraction with acetic acid and passing it through a cationic exchange column for chromatographic analysis. However, there are other results that contradict TTX as the main active ingredient, given that the presence of neurotoxins in local fish and amphibians of the Caribbean continues not to be recognized in chromatographic analyses12. It is also possible to find high concentrations of TTX and its analogues 4-epiTTX and 4,9-anhidroTTX in cooked puffer fish using fluorescence detection and chromatography17. This inability to discriminate between active and inactive components, without recognizing who the real toxic elements really are, suggests that chemical analyzes and toxicological studies must be carried out on each ingredient individually. Later the studies would be done as combinations of ingredients contained in these voodoo potions. This voodoo drug acts relatively similar to ketamine, tiletamine, dextromethorphan, and phencyclidine (PCP), the latter being a very toxic NMDA receptor antagonist drug22 commonly known as “Angel Dust”, “Peace Pill” or “Weed” (when consumed in combination with marijuana). PCP and TTX are capable of producing hallucinogenic effects and paralysis by blocking ion, potassium and sodium channels, respectively23. High concentrations of PCP induce the release of [3H]dopamine from cultures of dissociated rat midbrain cells, being independent of Ca2+ and insensitive to TTX24. TTX alone has no effect on the spontaneous release of [3H]dopamine24. Many of these hallucinations are also attributed to epileptic seizures, where they have a historical association with religion, mainly through the concept of spirit possession25.
Bufotenine as another ritual ingredient
The film describes a poisonous marine toad, which could be the same “giant toad”, “cane toad” or “marine toad” (Bufo marinus, also know as Rhinella marina), being a species of anuran amphibian of the family Bufonidae. One of the chemicals excreted by this toad is bufotenin26, classified as a drug of the same classification as heroin and cocaine. Wade Davis himself published an anthropological article where he hypothesizes that for a long time the ancient people of Mesoamerica used Bufo marinus as a ritual intoxicant26, but this toad is also rejected as a candidate for such use due to the toxicity of its venom, being another candidate most likely the Sonoran Desert toad, Bufo alvarius, which secretes large amounts of the potent hallucinogen 5-methoxy-N,N-dimethyltryptamine (5-MeO-DMT). Although the venom of B. alvarius is toxic when consumed orally, it can be smoked safely and is powerfully psychoactive by that route of administration, giving rise to a hallucinogenic and psychoactive agent, known as the “God molecule”, which could have been used by pre-Columbian peoples of the New World26. The hallucinogenic effects of bufotenine are believed to last less than an hour, showing activity similar to that of LSD and other known hallucinogens (psilocin and 5-MeO-DMT) at the putative hallucinogenic serotonin (5-HT) receptors, 5-HT2A and 5-HT2C27. The binding and activation of hallucinogenic receptors does not have a complete scope, this evidences the idea that the lack of the classic hallucinogenic response of the drug in experiments with humans is due to the poor ability to cross the blood-brain barrier27. It is known that certain serious mental disorders such as schizophrenia and autism spectrum disorders (ASD) are associated with the endogenous synthesis and urinary excretion of a psychomimetic molecule bufotenine (NN-dimethyl-5-hydroxytryptamine)28, 29, a product of the serotonin degradation pathway. Therefore, the presence and levels of bufotenin could be useful and important markers of some psychiatric disorders.
Conclusions
The myth of the living dead due to the voodoo zombie drug is considered an intoxication by neurotoxic drugs that must be well evaluated with the appropriate tools, such as the use of evoked potentials to rule out an erroneous diagnosis of brain death. The catalepsy or apparent death of a patient due to the voodoo drug is well established in the scientific literature due to the high concentrations of TTX, a powerful paralyzing and hypotensive neurotoxin of certain species of puffer fish native to Haiti. Given the impossibility of effective treatment, a life support system such as ventilation, hemodialysis for plasma clearance, hydration and gastric lavage with activated charcoal is advisable. Neostigmine treatment remains inconclusive.
References
1. Davis W. La Serpiente y el Arco Iris: Historia secreta de la magia, los zombis y el vudú. Buenos Aires, Argentina: Emece Editores; 1985.
2. Gorelik O, Feldman L, Cohen N. Heart failure and orthostatic hypotension. Heart Fail. Rev. 2016;21(5):529-538.
3. Memmer MK. Acute orthostatic hypotension. Heart Lung. 1988;17(2):134-143.
4. Rozenberg J, Wieling W, Schon IK, Westerhof B, Frampton C, Jardine D. MSNA during prolonged post-faint hypotension. Clin. Auton. Res. 2012;22(4):167-173.
5. De Ryck M, Teitelbaum P. Morphine catalepsy as an adaptive reflex state in rats. Behav. Neurosci. 1984;98(2):243-261.
6. Escalante-Cobo JL. Muerte encefálica. Evolución histórica y situación actual. Med. Intensiva. 2000;24:97-105.
7. Guidelines for the determination of death. Report of the medical consultants on the diagnosis of death to the President’s Commission for the Study of Ethical Problems in Medicine and Biomedical and Behavioral Research. JAMA. 1981;246(19):2184-2186.
8. Hills TE. Determinación de la muerte cerebral Revisión de las directrices basadas en la evidencia. Nursing. 2011;29(3):16-22.
9. Martínez-Martín P, Martínez Sarriés FJ. Actividad motora espontánea y refleja en la muerte cerebral [Spontaneous and reflex motor behavior in brain death]. Neurologia. 1994;9(9):407-409.
10. Escudero-Augusto D. Diagnóstico clínico de muerte encefálica. Prerrequisitos y exploración neurológica. Med. Intensiva. 2000;24:106-15.
11. Paniagua-Soto J, Piñero-Benítez M. Muerte encefálica: ¿cuál es el valor diagnóstico de los potenciales evocados multimodales? Med. Intensiva. 2000;24:124-34.
12. Craan AG. Toxicologic aspects of voodoo in Haiti. Biomed. Environ. Sci. 1988;1(4):372-381.
13. Davis EW. The ethnobiology of the Haitian zombi. J. Ethnopharmacol. 1983;9(1):85-104.
14. Chen R, Chung SH. Mechanism of tetrodotoxin block and resistance in sodium channels. Biochem. Biophys. Res. Commun. 2014;446(1):370-374.
15. Borison HL, McCarthyle, Clark WG, Radhakrishan N. Vomiting, hypothermia, and respiratory paralysis due to tetrodotoxin (puffer fish poison) in the cat. Toxicol. Appl. Pharmacol. 1963;5:350-357.
16. Ahasan HA, Mamun AA, Karim SR, Bakar MA, Gazi EA, Bala CS. Paralytic complications of puffer fish (tetrodotoxin) poisoning. Singapore Med. J. 2004;45(2):73-74.
17. Islam QT, Razzak MA, Islam MA, et al. Puffer fish poisoning in Bangladesh: clinical and toxicological results from large outbreaks in 2008. Trans. R. Soc. Trop. Med. Hyg. 2011;105(2):74-80.
18. Bucciarelli GM, Lechner M, Fontes A, Kats LB, Eisthen HL, Shaffer HB. From Poison to Promise: The Evolution of Tetrodotoxin and Its Potential as a Therapeutic. Toxins. 2021;13(8):517.
19. Liu SH, Tseng CY, Lin CC. Is neostigmine effective in severe pufferfish-associated tetrodotoxin poisoning? Clin. Toxicol. (Phila). 2015;53(1):13-21.
20. Magarlamov TY, Melnikova DI, Chernyshev AV. Tetrodotoxin-Producing Bacteria: Detection, Distribution and Migration of the Toxin in Aquatic Systems. Toxins. 2017;9(5):166.
21. Benedek C, Rivier L. Evidence for the presence of tetrodotoxin in a powder used in Haiti for zombification. Toxicon. 1989;27(4):473-480.
22. Näkki R, Koistinaho J, Sharp FR, Sagar SM. Cerebellar toxicity of phencyclidine. J. Neurosci. 1995;15(3 Pt 2):2097-2108.
23. Aguayo LG, Albuquerque EX. Phencyclidine blocks two potassium currents in spinal neurons in cell culture. Brain Res. 1987;436(1):9-17.
24. Mount H, Boksa P, Chaudieu I, Quirion R. Phencyclidine and related compounds evoked [3H]dopamine release from rat mesencephalic cell cultures by a mechanism independent of the phencyclidine receptor, sigma binding site, or dopamine uptake site. Can. J. Physiol. Pharmacol. 1990;68(9):1200-1206.
25. Carrazana E, DeToledo J, Tatum W, Rivas-Vasquez R, Rey G, Wheeler S. Epilepsy and religious experiences: Voodoo possession. Epilepsia. 1999; 40(2): 239-241.
26. Weil AT, Davis W. Bufo alvarius: a potent hallucinogen of animal origin. J. Ethnopharmacol. 1994;41(1-2):1-8.
27. McBride MC. Bufotenine: toward an understanding of possible psychoactive mechanisms. J. Psychoactive Drugs. 2000;32(3):321-331.
28. Emanuele E, Colombo R, Martinelli V, et al. Elevated urine levels of bufotenine in patients with autistic spectrum disorders and schizophrenia. Neuro Endocrinol. Lett. 2010;31(1):117-121.
29. Takeda N, Ikeda R, Ohba K, Kondo M. Bufotenine reconsidered as a diagnostic indicator of psychiatric disorders. Neuroreport. 1995;6(17):2378-2380.

Carmen María Fernandez-Martos. Graduate in Biology from the University of Jaén, PhD in Chemistry from the University of Castilla-La Mancha, and specialist in Biochemistry, Molecular Biology and Biomedicine from the Autonomous University of Madrid. Currently, she is a professor of Pharmacology at the Faculty of Pharmacy and Health Sciences of the CEU-San Pablo University, where she also directs a research laboratory, “METBRAIN”, focused on studying the pathological mechanisms responsible for metabolic dysfunction of the adipose tissue, and leptin, in neurodegenerative pathologies such as Amyotrophic Lateral Sclerosis (ALS) and Frontotemporal Dementia (FTD).

Nora Suleiman-Martos. PhD in Psychology from the University of Granada. She is currently an associate professor at the Faculty of Health Sciences of the University of Granada, where she teaches associated with the same department using a gamification methodology and teaching innovation resources, including the use of Cinema as a teaching educational resource. Her line of research focuses on the field of public health and psychosocial problems in the health field.

José Luis Gómez-Urquiza. PhD in Psychology from the University of Granada. He is currently an Associate professor of Nursing at the Faculty of Health Sciences of Ceuta of the University of Granada, where he teaches teaching associated with the same department using a gamification methodology, game-based learning and teaching innovation resources, including the use of escape room as a teaching educational resource. His line of research focuses on the field of health.

Isabel Prieto Gómez. Full professor of Physiology at the Department of Health Sciences. Faculty of Experimental Sciences of the University of Jaén. Head of the Endocrinology and Nutrition research group at the University of Jaén (Neuroendocrinology and Nutrition, BIO-221).

Manuel Ramírez Sánchez. Full professor of Physiology at the Department of Health Sciences. Faculty of Experimental Sciences of the University of Jaén. Head of the PAI CVI-221 research group (Peptides and Peptidases).

Ana Belén Segarra Robles. PhD in Biological Sciences from the University of Jaén. She is an associate professor at the University of Jaén and an active member of the BIO-221 group (Neuroendocrinology and Nutrition).

Francisco José García Cózar. Full professor of Immunology at the Department of Biomedicine, Biotechnology and Public Health of the University of Cádiz. He holds a doctorate from the University of Córdoba with the thesis “Functional study of molecules involved in the activation of human T cells.” Head of the CTS-498 research group (Functional Genomics of the Immune System. Immunological Alteration of Reproduction and Anesthesia).

Germán Domínguez-Vías. PhD in Health Sciences from the University of Cádiz and PhD in Food Safety from the University of Jaén. He is currently an Associate professor at the Faculty of Health Sciences (Ceuta Campus) of the University of Granada, where he teaches teaching associated with the department of physiology in the nursing degree, and implements Cinema as an educational resource within the curriculum. His line of research focuses on neurodegeneration and blood pressure regulation.