eISSN 2444-7986
DOI: https://doi.org/10.14201/orl.33057
REVIEW ARTICLE
SYSTEMATIC REVIEW OF PLATYSMA MYOCUTANEOUS FLAP IN ORAL CANCER RECONSTRUCTION
Revisión sistemática del colgajo miocutáneo de platisma en la reconstrucción de cáncer oral
María SAN MILLÁN-GONZÁLEZ ; Luis Miguel TORRES-MORIENTES
; Luis Miguel TORRES-MORIENTES ; Marta ALONSO-MESONERO
; Marta ALONSO-MESONERO ; Jaime SANTOS-PÉREZ
; Jaime SANTOS-PÉREZ
Otorhinolaryngology-Head and Neck Surgery Department, Clinic University Hospital, Valladolid, Spain.
Correspondence: msanmillang@saludcastillayleon.es
Reception date: February 9, 2025
Date of Acceptance: April 18, 2025
Publication date: May 22, 2025
Date of publication of the issue: June 27, 2025
Conflict of interest: The authors declare no conflicts of interest
Images: The authors declare that the images have been obtained with the permission of the patients
Rights policy and self-archive: the self-archive of the post-print version (SHERPA / RoMEO) is allowed
License CC BY-NC-ND. Creative Commons Attribution-Noncommercial-NoDerivate Works 4.0 International
University of Salamanca. Its commercialization is subject to the permission of the publisher
SUMMARY: Introduction and objective: Oral cavity reconstruction requires effective techniques to restore both functionality and aesthetics; this review evaluates the outcomes of platysma myocutaneous flaps (PMF).
Method: A systematic review with a narrative synthesis approach was performed, analyzing clinical outcomes from primary research studies. PubMed, Embase, and Scopus databases were used. The search included terms such as «platysmal flap», «oral cancer», «reconstruction», and «clinical outcomes», targeting studies on PMF for buccal squamous cell carcinoma (BSCC). Articles in all languages were considered, excluding those focused on experimental or alternative flap techniques. Risk of bias was assessed using the ROBINS-I tool.
Results: PMF and local flaps achieved high success rates in function and aesthetics; 73–82 % of patients restored normal oral intake and speech; complications like partial necrosis (6.7–10 %) were managed conservatively.
Discussion: PMF proves a versatile, time-efficient solution for intraoral defects, particularly in settings where free tissue transfer is not feasible; outcomes were most favourable for smaller defects.
Conclusions: Regional flaps, especially PMF, are effective and practical for oral cavity reconstruction, offering excellent functional recovery, aesthetic results, and quality-of-life improvements with manageable complication rates.
KEYWORDS: platysmal flap; myocutaneous flap; oral cavity reconstruction; buccal squamous cell carcinoma; dermoplatysmal flap
RESUMEN: Introducción y objetivo: La reconstrucción de la cavidad oral requiere técnicas eficaces para restaurar la función y la estética; esta revisión evalúa los resultados de los colgajos miocutáneos de platisma (PMF).
Método: Se realizó una revisión sistemática con enfoque de síntesis narrativa, analizando resultados clínicos de estudios primarios, utilizando las bases de datos PubMed, Embase y Scopus. La búsqueda incluyó términos como «platysmal flap», «oral cancer», «reconstruction», y «clinical outcomes», centrada en estudios sobre colgajos miocutáneos de platisma para carcinoma escamoso bucal. Se consideraron artículos en todos los idiomas, excluyendo aquellos enfocados en técnicas experimentales o alternativas de colgajos. La evaluación del riesgo de sesgo se llevó a cabo mediante la herramienta ROBINS-I.
Resultados: Los colgajos PMF y locales lograron altas tasas de éxito en función y estética; entre el 73 % y el 82 % de los pacientes recuperaron la ingesta oral normal y el habla. Complicaciones como la necrosis parcial (6.7–10 %) se manejaron de forma conservadora.
Discusión: Los PMF resultan ser una solución versátil y eficiente en tiempo para defectos intraorales, especialmente en entornos donde la transferencia de tejido libre no es viable; los mejores resultados se observaron en defectos pequeños.
Conclusiones: Los colgajos regionales, especialmente los PMF, son efectivos y prácticos para la reconstrucción de la cavidad oral, ofreciendo una excelente recuperación funcional, resultados estéticos y mejoras en la calidad de vida, con tasas de complicaciones manejables.
PALABRAS CLAVE: colgajo de platisma; colgajo miocutáneo; reconstrucción de cavidad oral; carcinoma escamoso bucal
INTRODUCTION
The platysma myocutaneous flap (PMF), is a versatile yet underutilized technique in head and neck reconstructive surgery, especially for intraoral and maxillofacial defects caused by trauma or oncological resection [1-3]. First described by Futrell et al. in 1978, the PMF offers several advantages, including a thin, pliable structure, proximity to the defect site, minimal donor site morbidity, and the ability to achieve primary neck closure [1, 2].
Despite extensive literature on flap techniques in head and neck reconstruction, only three studies focus specifically on the PMF, underscoring a surprising gap in exploring its functional and aesthetic benefits, as well as its simplicity and accessibility [1-3]. The PMF is particularly effective for small to medium-sized oral cavity defects, offering functional restoration and cosmetic satisfaction with lower complication rates. Reported challenges, such as partial necrosis, dehiscence, and venous congestion (18–45 % in some studies), can be minimized with meticulous surgical planning, including preserving the external jugular vein [2].
This review aims to identify studies on the use of myocutaneous flaps in reconstructing defects caused by oral cancer, particularly buccal squamous cell carcinoma, analyzing clinical outcomes, surgical results, and complications.
MATERIAL AND METHODS
A systematic review of the literature with a narrative synthesis approach was performed using the PubMed, Embase, and Scopus databases. Exclusively primary research sources reporting clinical data on platysma myocutaneous flaps were included. The search strategy included the following terms: ("platysmal flap"[Title/Abstract] OR "myocutaneous flap"[Title/Abstract] OR "cervical flap"[Title/Abstract]) AND ("buccal carcinoma"[Title/Abstract] OR "buccal squamous cell carcinoma"[Title/Abstract] OR "oral cancer"[Title/Abstract] OR "head and neck cancer"[Title/Abstract] OR "oral cavity cancer"[Title/Abstract]) AND ("reconstruction"[Title/Abstract] OR "surgical reconstruction"[Title/Abstract] OR "oral defect reconstruction"[Title/Abstract]) AND ("clinical outcomes"[Title/Abstract] OR "surgical outcomes"[Title/Abstract] OR "complications"[Title/Abstract] OR "case series"[Title/Abstract]).
The inclusion criteria were as follows: (1) original research on the use of platysma myocutaneous flaps for BSCC, (2) clinical studies with reported outcomes, and (3) published within the last 10 years. Articles were included without language restrictions. Studies focusing solely on other flap techniques or experimental studies without clinical application were excluded. Data were extracted on patient demographics, defect characteristics, surgical technique, postoperative outcomes, and complications. Two independent reviewers screened the articles, and discrepancies were resolved by consensus. A PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) 2020 flow diagram detailing the study selection process is provided [4] (Figure 1). The methodological quality of the included non-randomized studies was assessed using the ROBINS-I (Risk Of Bias In Non-randomized Studies of Interventions) tool. Each study was evaluated across seven domains. Overall risk of bias was classified as low, moderate, or serious, based on the cumulative assessment.
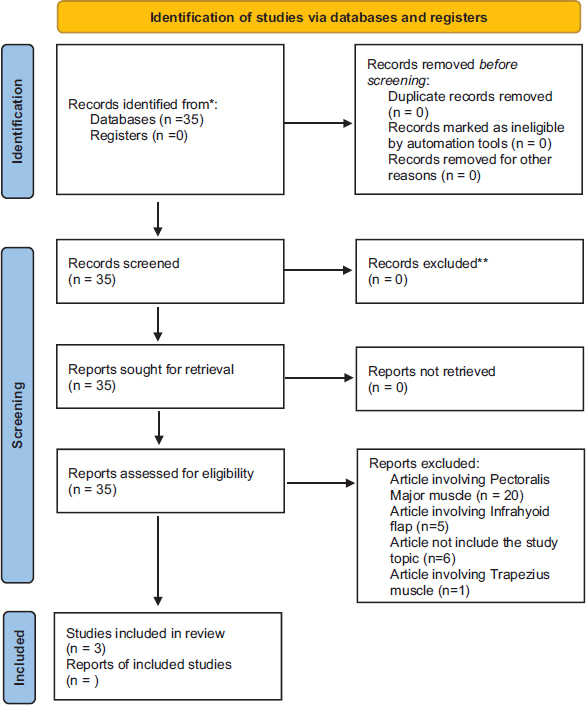
Figure 1. PRISMA 2020 flow diagram for new systematic reviews which included searches of databases and registers only.
RESULTS
As shown in the PRISMA flow diagram, the described methodology resulted in 35 articles [4]. Following the detailed screening process, three studies were selected: one retrospective study, one prospective study, and one case series. We created a table specifying the authors, country, year of publication, study type, and the main results analyzed (Table 1). While there are numerous articles addressing flaps for oral cavity defect reconstruction, we have chosen to focus exclusively on platysma myocutaneous flaps, which explains the limited number of articles selected. The risk of bias of the included studies was evaluated using the ROBINS-I tool. One study (Humne et al.) presented a moderate risk of bias due to limitations in confounding control and subjective outcome measures [1]. The case series by Sahni et al. showed a serious overall risk due to small sample size, lack of comparator, and unclear reporting [2]. The retrospective study by Joshi et al. was rated as moderate risk [3] (Table 2).
Table 1. Table of results in order of appearance in the article.
Study |
Year and country |
Study type |
Patients |
Age range |
Gender |
Diagnosis |
Location |
Treatment |
Surgical duration |
Postoperative managment |
Complications |
Follow-up |
ROBINS-I Risk of Bias |
Humne A et al. [1] |
India, 2024 |
Prospective |
30 |
Not specified |
Not specified |
Oral cancer |
Oral cavity |
Wide local excision and PMF reconstruction |
Not specified (flap harvesting <15 min.) |
Regular wound care, pain management |
26.67 % infection, 16.67 % dehiscence, 6.77 % necrosis |
1 week, 1, 3, and 6 months |
Moderate |
Sahni M. et al. [2] |
India, 2023 |
Case series |
10 |
24-42 years |
Male |
Squamous cell carcinoma and nodular leukoplakia |
Buccal mucosa, floor of mouth |
Wide local excision and PMF reconstruction |
Not specified |
Prolonged nasogastric nutrition (15 days) in 2 cases |
10 % partial necrosis, 10 % donor site necrosis |
Not specified |
Serious |
Joshi P. et al. [3] |
India, 2024 |
Retrospective |
104 (4 PMF) |
25-75 years |
6:1 (M:F) |
Squamous cell carcinoma |
Buccal mucosa, floor of mouth, tongue and lip |
Local flaps: 4 PMF |
45-70 mins. |
Nasogastric nutrition (12 days) |
Partial necrosis (n=1) |
6 months |
Moderate |
(PMF= platysma myocutaneous flaps)
Table 2. Risk of bias was assessed according to the ROBINS-I (Risk of Bias In Non-randomized Studies - of Interventions) tool.
Study |
Confounding |
Selection of participants |
Classification of interventions |
Deviations from intended interventions |
Missing data |
Measurement of outcomes |
Selection of reported result |
Overall Risk |
Humne et al. [1] |
Moderate |
Low |
Low |
Low |
Low |
Moderate |
Low |
Moderate |
Sahni et al. [2] |
Serious |
Moderate |
Low |
Low |
Moderate |
Serious |
Moderate |
Serious |
Joshi et al. [3] |
Moderate |
Low |
Low |
Low |
Low |
Moderate |
Low |
Moderate |
DISCUSSION
PATIENT DEMOGRAPHICS AND STUDY CHARACTERISTICS
Three studies, collectively involving 144 patients, examined reconstruction for oral cavity defects. These included a prospective analysis of 30 patients utilizing platysma myocutaneous flaps (PMF) for oral and maxillofacial reconstruction, a retrospective review of 104 cases treated with local flap reconstructions (including 4 PMF cases), and a case series of 10 patients focusing on PMF for intraoral defects [1-3]. Patient ages ranged from 24 to 75 years, with a predominance of males. The male-to-female ratio in the retrospective cohort was 6:1, and the case series included exclusively male participants. Most cases involved squamous cell carcinoma (SCC) at varying stages, with some studies also addressing premalignant lesions, such as nodular leukoplakia [1-3].
SURGICAL TECHNIQUES AND TREATMENT MODALITIES
All studies employed regional or local flaps for reconstruction. The prospective analysis emphasized the PMF technique, noting an average harvesting time of under 15 minutes [1]. The retrospective review incorporated melolabial, supraclavicular, submental, and islanded facial artery myomucosal (FAMM) flaps, while the case series solely investigated PMF, highlighting its effectiveness in managing intraoral defects [2, 3]. Surgical times varied, with local flap procedures requiring 45–70 minutes, influenced by complexity, and PMF reconstruction adding minimal time beyond neck dissection [1-3].
OUTCOMES AND SUCCESS RATES
Functional and aesthetic outcomes were positive across all studies. In the prospective study, oral function and aesthetics improved significantly, as measured by the University of Washington Quality of Life questionnaire (UW-QOL). Six months postoperatively, 73.3 % of patients reported no swallowing difficulties, 76.7 % had normal taste perception, and all maintained intelligible speech, though some required repetition early in recovery [1].
The retrospective review revealed that 82.7 % of patients achieved normal oral intake, and 80.8 % retained clear speech with minimal repetition, as assessed by the Performance Status Scale for Head and Neck Cancer (PSS-HN). Outcomes were particularly favorable for small- to medium-sized defects, with the melolabial flap achieving high success rates [3].
The case series demonstrated satisfactory cosmetic and functional outcomes in 80 % of patients, underscoring PMF’s utility for intraoral reconstruction, especially in resource-constrained settings or when free tissue transfer was contraindicated [2].
COMPLICATIONS
Complication rates varied across studies. The prospective analysis reported infection (26.7 %), flap dehiscence (16.7 %), and partial necrosis (6.7 %), all managed conservatively without secondary interventions. Shoulder stiffness affected 20 % of patients at one week but resolved completely by six months [1].
In the retrospective cohort, partial necrosis was reported in only one PMF case, translating to a low complication rate for this technique. Total flap loss was noted in 1.9 % of cases across all flap types. Donor site complications, such as wound gaping and seroma formation, occurred in 5.8 % of patients and were managed conservatively. Notably, the supraclavicular flap demonstrated the highest complication rate among the local flaps studied. [3].
The case series documented partial necrosis and donor site skin loss in 10 % of patients each. One instance of complete flap loss healed by secondary intention, with all other complications managed conservatively without significant long-term effects [2].
POSTOPERATIVE MANAGEMENT AND RECOVERY
Postoperative care protocols varied across studies. In the prospective study, pain management and wound care were emphasized, resulting in 96.7 % of patients being pain-free and fully resuming daily activities by six months [1]. In the retrospective cohort, nasogastric feeding tubes were maintained for an average of 12 days, and tracheostomy tube corking was initiated by postoperative day five in 13.5 % of cases [3]. For the case series, nasogastric nutrition was required for up to 15 days in patients with complications [2].
Although the included studies reported favorable clinical outcomes, the ROBINS-I assessment indicated moderate to serious risk of bias, especially in relation to confounding and measurement domains. These factors should be considered when interpreting the overall evidence.
These findings highlight the efficacy and safety of local and regional flap techniques, particularly PMF, for reconstructing oral cavity defects while achieving favorable functional, cosmetic, and quality-of-life outcomes.
CONCLUSIONS
The analysed studies demonstrate that platysma myocutaneous flaps, are effective options for reconstructing oral cavity defects, offering favourable functional and aesthetic outcomes. PMF is a reliable choice, especially in resource-limited settings or for patients contraindicated for free tissue transfer. While complication rates vary, most issues are manageable conservatively with minimal long-term sequelae. These techniques support optimal recovery of oral intake, speech intelligibility, and quality of life, underscoring their clinical value in oral and maxillofacial reconstruction.
REFERENCES
1.Humne A, Agarwal R, Uppal A, Mehra R, Gupta H, Mehra H. Efficacy and Functional Outcomes of Platysma Myocutaneous Flap in Oral and Maxillofacial Reconstruction. Cureus. 2024 Sep 29;16(9):e70464. https://doi.org/10.7759/cureus.70464. PMID: 39479141; PMCID: PMC11522030.
2.Sahni M, Singh S, Kishor K, Patel P, Sharma R. Platysmal Myocutaneous Flap for Intra Oral Defects:Is It an Underutilized Option? Our Experience of 10 Cases. Indian J Otolaryngol Head Neck Surg. 2023 Dec;75(4):3581-3584. https://doi.org/10.1007/s12070-023-04055-y. Epub 2023 Jul 10. PMID: 37974677; PMCID: PMC10645692.
3.Joshi P, Bavaskar M, Shetty R, Singh A, Nair S, Chaturvedi P. Local Flap Reconstructions in Oral Cavity Defects: An Insight from 104 Cases. Rambam Maimonides Med J. 2024 Jul 30;15(3):e0012. https://doi.org/10.5041/RMMJ.10526. PMID: 39088704; PMCID: PMC11294683.
4.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. https://doi.org/10.1136/bmj.n71