eISSN 2444-7986
DOI: https://doi.org/10.14201/orl.32778
CASE REPORT
DERMOPLATYSMAL FLAP RECONSTRUCTION FOLLOWING BUCCAL SQUAMOUS CELL CARCINOMA RESECTION
Reconstrucción con colgajo dermoplatismal tras resección de carcinoma escamoso bucal
María SAN MILLÁN-GONZÁLEZ ; Luis Miguel TORRES-MORIENTES
; Luis Miguel TORRES-MORIENTES ; Marta ALONSO-MESONERO
; Marta ALONSO-MESONERO ; Jaime SANTOS-PÉREZ
; Jaime SANTOS-PÉREZ
Otorhinolaryngology-Head and Neck Surgery Department, Clinic University Hospital, Valladolid, Spain.
Correspondence: msanmillang@saludcastillayleon.es
Reception date: January 11, 2025
Date of Acceptance: April 6, 2025
Publication date: May 23, 2025
Date of publication of the issue: June 27, 2025
Conflict of interest: The authors declare no conflicts of interest
Images: The authors declare that the images have been obtained with the permission of the patients
Rights policy and self-archive: the self-archive of the post-print version (SHERPA / RoMEO) is allowed
License CC BY-NC-ND. Creative Commons Attribution-Noncommercial-NoDerivate Works 4.0 International
University of Salamanca. Its commercialization is subject to the permission of the publisher
SUMMARY: Introduction and objective: Squamous cell carcinoma (SCC) of the buccal mucosa is an aggressive malignancy requiring extensive resections and reconstruction. The dermoplatysmal flap is a reliable option for restoring function and aesthetics. This report evaluates its effectiveness in complex cases. Description: An 81-year-old male with HPV-positive SCC underwent tumor excision, maxillary shaving, and selective neck dissection. A dermoplatysmal flap was used for reconstruction. Recovery was uneventful, with no recurrence at 18 months.
Discussion: The dermoplatysmal flap offers robust vascularity, functional restoration, and aesthetic outcomes. Its versatility makes it ideal for large oral defects, ensuring durable results.
Conclusions: The dermoplatysmal flap is a valuable reconstructive option, ensuring oncological control, functional recovery, and aesthetic satisfaction in SCC cases.
KEYWORDS: buccal carcinoma; dermoplatysmal flap; HPV; oral reconstruction; squamous cell carcinoma.
RESUMEN: Introducción y objetivo: El carcinoma escamoso de mucosa bucal es una neoplasia agresiva que requiere resecciones extensas y reconstrucción. El colgajo dermoplatismal se presenta como una opción fiable para restaurar la función y la estética. Este caso evalúa su eficacia en casos complejos. Descripción: varón de 81 años con carcinoma escamoso positivo para VPH fue sometido a excisión tumoral, afeitado maxilar y disección selectiva del cuello. Se utilizó un colgajo dermoplatismal para la reconstrucción. La recuperación fue favorable, sin recurrencia a los 18 meses. Discusión: El colgajo dermoplatismal ofrece gran vascularización, restauración funcional y resultados estéticos. Su versatilidad lo hace ideal para grandes defectos orales, garantizando resultados duraderos. Conclusiones: El colgajo dermoplatismal es una técnica reconstructiva eficaz, asegurando control oncológico, recuperación funcional y satisfacción estética.
PALABRAS CLAVE: carcinoma bucal; colgajo dermoplatismal; VPH; reconstrucción oral; carcinoma de células escamosas.
INTRODUCTION
Squamous cell carcinoma (SCC) of the buccal mucosa is a particularly aggressive malignancy, characterized by its potential for local invasion and regional metastasis [1]. Management often involves extensive surgical resection to achieve oncological control, which frequently results in significant defects and functional impairment [1, 2]. Such defects, especially in the oral cavity, pose challenges to the restoration of essential functions like speech, mastication, and deglutition, while also impacting aesthetics and quality of life [3].
Reconstructive techniques play a critical role in addressing these challenges. The dermoplatysmal flap has gained prominence as a reliable option for covering large defects [4]. This technique offers several advantages, including robust vascularity, pliability, and ease of harvest, allowing effective restoration of both functionality and appearance. Its versatility makes it particularly suited for complex oral reconstructions, ensuring durable outcomes while minimizing donor site morbidity [4, 5]. By combining oncological safety with functional and aesthetic recovery, the dermoplatysmal flap is increasingly recognized as an optimal reconstructive solution in cases of buccal SCC [4].
DESCRIPTION
An 81-year-old male presented with a lesion on the right buccal mucosa, initially evaluated in our hospital's otorhinolaryngology department (Figure 1A). A biopsy was performed, and histopathological analysis confirmed a neoplastic epithelial malignancy exhibiting moderate atypia, cellular pleomorphism, nuclear hyperchromasia, and frequent mitotic figures. There were signs of keratinisation, including intercellular bridges and frequent keratin pearls. The neoplasm infiltrated the lamina propria, with desmoplastic reaction and a patchy lymphoplasmacytic infiltrate. On the surface, there were verruciform areas with binucleation and paranuclear vacuoles, interpreted as koilocytic atypia.
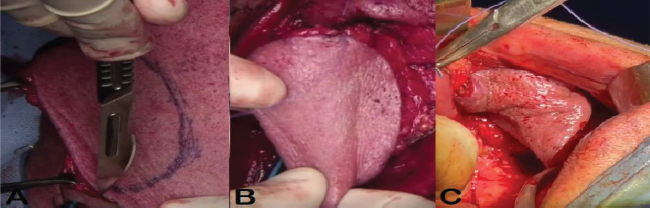
Figure 1. A: Lesion on the right buccal mucosa at diagnosis. B: Immediate postoperative view of the dermoplatysmal flap. C: Follow-up view of the dermoplatysmal flap.
Immunohistochemical staining demonstrated p16 positivity, corroborating the diagnosis of HPV-associated well-differentiated squamous cell carcinoma (SCC).
Further imaging via CT of the neck and thorax revealed a tumour in the right buccal mucosa, measuring approximately 42 x 14 x 27.5 mm, with potential invasion of the gingival mucosa and questionable involvement of the external maxillary cortex. Additionally, involvement of the retromolar trigone and anterior portion of the medial pterygoid muscle was noted. There was asymmetry of the tonsillar pillars and mild medialisation of the vocal cords. Cervical and submandibular lymphadenopathy were observed, but no significant vascular abnormalities were identified. A thoracic CT showed no significant mediastinal or hilar adenopathy, although the presence of chronic fibrotic changes and bronchiectasis were noted. A previously known 40 mm aneurysmal dilation of the ascending aorta was stable, and pleural effusion was minimal. The patient had no evidence of metastatic disease.
The patient also underwent magnetic resonance imaging (MRI) to further evaluate the extent of tumour invasion. However, due to the presence of local artefacts, assessment of the oral cavity and buccal region was suboptimal. Despite this limitation, the posterior aspect of the known tumour in the right buccal mucosa was visualised, showing loss of the plane of separation from the pterygoid musculature, confirming tumour infiltration. STIR sequences demonstrated increased signal intensity and thickening of the right tonsillar pillar, associated with thinning of the parapharyngeal fat triangle, suggesting direct spread of the tumour to the tonsillar region. Post-contrast sequences, including perfusion, did not provide further useful information due to artefacts. Cervical lymph nodes were indeterminate on MRI, further necessitating physical examination and biopsy for conclusive assessment.
The patient underwent a transoral surgical excision of the tumour using a Feyh-Kastenbauer (FK) retractor (Gyrus Medical Inc, Tuttlingen, Germany) to optimise exposure of the posterior oral cavity and retromolar trigone. Resection included wide local excision with oncological margins, followed by high-speed burr shaving of the right posterior maxillary alveolar ridge to ensure clearance of suspected bony involvement. A selective neck dissection of levels I–III was performed on the right side (selective cervical lymphadenectomy), with identification and preservation of critical neurovascular structures. For soft tissue reconstruction, a right-sided dermoplatysmal advancement flap was mobilised and rotated into the surgical defect, allowing tension-free closure and restoration of mucosal continuity. Haemostasis was meticulously secured, and layered closure was performed. The postoperative course was uneventful (Figures 1B, 1C, and 2).
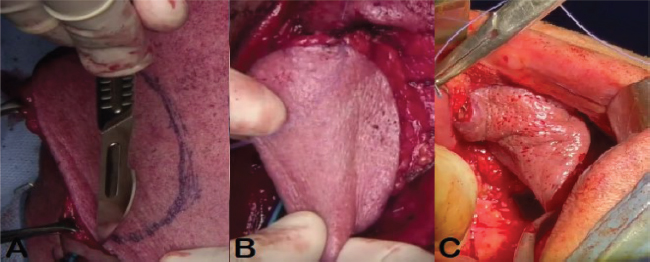
Figure 2. A: Incision with visible preoperative markings. B: Flap fully mobilised before insertion into the recipient area. C: Flap sutured after tumour excision.
Final pathology described a keratinising, conventional-pattern, well-differentiated (C1) SCC, measuring 2.5 x 2.3 x 1.7 cm, situated on the right buccal mucosa near the retromolar trigone, extending to the upper gingival mucosa, with an exophytic and infiltrative growth pattern. The tumour invaded the oral mucosa, reaching the striated muscle, and displayed an infiltrative growth front with a marked inflammatory response. The worst pattern of invasion (WPOI < 5) was noted in the central axis of the tumour, where tumour microfoci were detected more than 1 mm from the main tumour mass. Foci of comedonecrosis were also present. Importantly, no evidence of lymphovascular or perineural invasion was observed. The depth of invasion (DOI) was measured at 8 mm, and the tumour was staged as pT2, pN0. Given the pathological and clinical findings, the multidisciplinary tumour board deemed that no adjuvant treatment was necessary, a decision supported by current evidence-based guidelines.
The patient's postoperative recovery was favourable. He was closely monitored in follow-up consultations every six months. At one and a half years after surgery, the patient remains free of recurrence, with no signs of local or regional disease on clinical or radiological evaluation (Figure 1C). The ongoing follow-up aims to ensure early detection of any potential recurrence, which is crucial in cases of head and neck cancers.
DISCUSSION
Squamous cell carcinoma (SCC) of the oral cavity is among the most prevalent malignancies of the head and neck, particularly in the elderly population [1]. Its clinical course is often marked by significant morbidity due to local tissue invasion and the potential for regional and distant metastasis [1, 2]. A subset of these tumours is associated with high-risk human papillomavirus (HPV), especially HPV-16, which is known to confer a more favourable prognosis due to enhanced treatment responsiveness [1].
Histopathological findings such as keratinisation, koilocytic atypia, and overexpression of p16—a reliable surrogate marker for transcriptionally active HPV—support the diagnosis of HPV-related SCC. These features are typically associated with a well-differentiated tumour phenotype and may correlate with improved clinical outcomes. Nonetheless, in this case, the extensive local infiltration involving the retromolar trigone and the pterygoid musculature underscores the aggressive behaviour of the neoplasm despite its HPV-positive status [3].
Imaging modalities, particularly CT and MRI, are indispensable for accurate staging and surgical planning in oral SCC. In the present case, CT revealed a sizeable lesion with probable invasion of the maxillary cortex and surrounding musculature. MRI, although limited by local artefacts, confirmed infiltration into the pterygoid muscles and suggested involvement of adjacent anatomical compartments. Fortunately, there was no radiological evidence of major vascular invasion or distant metastasis, which favoured a surgical approach [4].
Reconstruction following oncologic resection of the oral cavity remains a critical step in restoring form and function [1-3]. The platysma myocutaneous flap (PMF) has re-emerged as a valuable reconstructive option, particularly in elderly or medically compromised patients where microvascular techniques may not be ideal. Humne et al. conducted a prospective study involving 30 patients treated with PMF reconstruction, demonstrating its versatility, low donor site morbidity, and acceptable complication profile—namely infection (26.7 %), flap dehiscence (16.7 %), and necrosis (6.77 %) [1]. In our case, postoperative recovery was uneventful, and the patient remained free of recurrence at 18 months, further supporting the reliability and efficacy of PMF in this context.
A broader retrospective series by Joshi et al., analysing 104 reconstructions with various local flaps, also included PMF in a minority (3.8 %) of cases, with good functional outcomes reported across subsites, including the buccal mucosa [3]. While the use of the FK (Feyh-Kastenbauer) retractor to facilitate transoral exposure is not specifically mentioned in these studies, our experience suggests it enhances surgical access and complements the use of PMF in confined oral spaces.
Additionally, Sahni et al. highlighted the cosmetic and functional advantages of PMF, especially its concealed donor site and ease of harvest [2]. In their cohort of 10 patients, only one case of total flap loss was reported, and most complications were minor and managed conservatively. These findings align closely with our experience, where the dermoplatysmal flap provided reliable soft tissue coverage, supported healing, and minimized functional deficits in the postoperative period [2–5].
Importantly, the multidisciplinary tumour board opted against adjuvant therapy based on a comprehensive assessment of pathological and clinical risk factors. The tumour was staged as pT2, pN0, with a depth of invasion of 8 mm, no perineural or lymphovascular invasion, and negative surgical margins. Although the tumour exhibited an infiltrative front and microfoci extending over 1 mm from the main mass (WPOI < 5), there was no extranodal extension or involvement of critical structures warranting adjuvant radiotherapy. The HPV-positive status—associated with enhanced radiosensitivity and improved prognosis—further reinforced a conservative approach [2, 3]. Thus, the decision to forego postoperative radiotherapy was consistent with current evidence-based guidelines and aligns with the principle of treatment de-intensification in selected low- to intermediate-risk HPV-related oral cavity cancers [1–5].
Finally, this case underscores the importance of comprehensive preoperative imaging despite technical limitations, as well as thoughtful flap selection tailored to tumour extent, patient comorbidities, and surgical expertise. The favourable oncological and functional outcomes observed reaffirm the role of the PMF as a valid alternative to free tissue transfer in selected oral cavity reconstructions.
CONCLUSIONS
This case underscores the intricate management of HPV-positive, well-differentiated SCC of the buccal mucosa, particularly in elderly patients. Despite the presence of extensive local invasion, surgical resection with clear margins remains the optimal treatment strategy. The use of advanced imaging techniques such as CT and MRI is crucial for assessing tumour extension and planning appropriate surgical interventions. Postoperative care, including reconstructive techniques, plays a vital role in preserving function and ensuring optimal recovery. Long-term surveillance for recurrence and metastasis is critical due to the high risk of local invasion and lymphatic dissemination.
REFERENCES
1. Humne A, Agarwal R, Uppal A, Mehra R, Gupta H, Mehra H. Efficacy and Functional Outcomes of Platysma Myocutaneous Flap in Oral and Maxillofacial Reconstruction. Cureus. 2024 Sep 29;16(9):e70464. https://doi.org/10.7759/cureus.70464. PMID: 39479141; PMCID: PMC11522030.
2. Sahni M, Singh S, Kishor K, Patel P, Sharma R. Platysmal myocutaneous flap for intraoral defects: is it an underutilized option? Our experience of 10 cases. Indian J Otolaryngol Head Neck Surg. 2023 Dec;75(4):3581–4. https://doi.org/10.1007/s12070-023-04055-y
3. Joshi P, Bavaskar M, Shetty R, Singh A, Nair S, Chaturvedi P. Local Flap Reconstructions in Oral Cavity Defects: An Insight from 104 Cases. Rambam Maimonides Med J. 2024 Jul 30;15(3):e0012. https://doi.org/10.5041/RMMJ.10526. PMID: 39088704; PMCID: PMC11294683.
4. Calabrese L, Fazio E, Bassani S, Abousiam M, Dallari V, Albi C, Nucera G, Nebiaj A, Zanghi F, Accorona R, Gazzini L. Systematic review of minimally-invasive reconstructive options for oral cavity defects. Acta Otorhinolaryngol Ital. 2024 May;44(Suppl 1):S42-S57. https://doi.org/10.14639/0392-100X-suppl.1-44-2024-N2904
5. Gosselin LE, Villemure-Poliquin N, Audet N. Quality of life after head and neck cancer surgery and free flap reconstruction: a systematic review. J Otolaryngol Head Neck Surg. 2024;53:19160216241248666. https://doi.org/10.1177/19160216241248666