eISSN 2444-7986
DOI: https://doi.org/10.14201/orl.32012
CASE REPORT
MYELITIS AND ANTI-YO ANTIBODIES: A PARANEOPLASTIC SYNDROME ASSOCIATED WITH NASOPHARYNGEAL CARCINOMA DETECTED BY POSITRON EMISSION TOMOGRAPHY. A CASE REPORT
Mielitis y anticuerpos anti-Yo: un síndrome paraneoplásico asociado al carcinoma nasofaríngeo detectado por tomografía por emisión de positrones. Descripción de un caso
Javier RIANCHO 1, 2, 3, 4; Eloy RODRÍGUEZ-RODRÍGUEZ
1, 2, 3, 4; Eloy RODRÍGUEZ-RODRÍGUEZ 1, 2, 3, 5; Andrea MARTÍNEZ-CAMERANO
1, 2, 3, 5; Andrea MARTÍNEZ-CAMERANO 6; Carmelo MORALES-ANGULO
6; Carmelo MORALES-ANGULO 2, 4, 6
2, 4, 6
1Department of Neurology Hospital General Sierrallana. Torrelavega. Spain
2Institute of Research Valdecilla (IDIVAL). Santander. Spain
3CIBERNED, Madrid, Spain
4Faculty of Medicine, University of Cantabria. Santander. Spain
5Department of Neurology. University Hospital Marqués de Valdecilla. Santander. Spain
6Department of Ear Nose and Throat. University Hospital Marqués de Valdecilla. Santander. Spain
Correspondence: carmelo.morales@unican.es
Reception date: March 16th, 2024
Date of Acceptance: October 1st, 2024
Publication date: October 4th, 2024
Date of publication of the issue: March 19th, 2025
Conflict of interest: The authors declare no conflicts of interest
Images: The authors declare that the images have been obtained with the permission of the patients
Rights policy and self-archive: the self-archive of the post-print version (SHERPA / RoMEO) is allowed
Licencia CC BY-NC-ND. Licencia Creative Commons Atribución-NoComercial-SinDerivar 4.0 Internacional
University of Salamanca. Its commercialization is subject to the permission of the publisher
SUMMARY: Introduction and objective: Paraneoplastic syndromes (PS) associated with nasopharyngeal carcinoma (NC) are very rare. We described a patient who presented with a paraneoplastic mielitis associated with anti-Yo antibodies and NC. Description: A 70 year-old previously healthy man presented with a progressive gait disorder. The diagnosis work up demonstrated both the presence of anti-Yo antibodies together with a NC, suspected by positron emission tomography (PET-CT). Despite prompt treatment with steroids, gammaglobulins and a satisfactory tumour therapy, partial neurological symptomathology persisted. Conclusions: Although rare, clinicians should consider the possibility of paraneoplastic aetiology when attending patients with NC presenting with subacute neurological symptoms.
KEYWORDS: paraneoplastic; myelitis; nasopharyngeal carcinoma; antiYo antibodies; Positron-Emission Tomography; head and neck carcinoma
RESUMEN: Introducción y objetivos: Los síndromes paraneoplásicos (SP) asociados al carcinoma nasofaríngeo (CN) son muy raros. Describimos a un paciente que presentó una mielitis paraneoplásica asociada con anticuerpos anti-Yo y CN. Descripción: Un hombre de 70 años previamente sano presentó un trastorno de la marcha progresivo. El estudio diagnóstico demostró la presencia de anticuerpos anti-Yo junto con un CN, sospechado por tomografía por emisión de positrones (PET-CT). A pesar del tratamiento rápido con esteroides, gammaglobulinas y una terapia tumoral satisfactoria, persistió una sintomatología neurológica parcial. Conclusiones: Aunque raro, los médicos deben considerar la posibilidad de etiología paraneoplásica al atender a pacientes con CN que presenten síntomas neurológicos subagudos.
PALABRAS CLAVE: paraneoplásico; mielitis; carcinoma nasofaríngeo; anticuerpos antiYo; Tomografía por Emisión de Positrones; carcinoma de cabeza y cuello
INTRODUCTION
Paraneoplastic syndromes (PS) are a varied group of cancer-related disorders arising from mechanisms other than metastases, metabolic or nutritional deficiencies, infections, or side effects of cancer treatments [1]. PS occur in 1-7.4 % of all cancer patients and may precede, follow, or coincide with the clinical manifestations of a malignant tumor [2].
Nasopharyngeal carcinoma (NC) is uncommon in Western countries but endemic in the southeastern parts of China. Risk factors for NC include tobacco use, hereditary predisposition, race, and, in cases of undifferentiated NC, Epstein-Barr virus (EBV) infection [3]. The most common presenting symptoms of NC are cervical lymphadenopathy, and ear and nasal problems [3]. However, a small group of patients may develop symptoms related to PS [4].
Various types of PS have been associated with NC, including connective tissue diseases (such as dermatomyositis and scleroderma), paraneoplastic endocrine syndromes (such as syndrome of inappropriate secretion of antidiuretic hormone - SIADH), paraneoplastic hematologic syndromes (like tumor fever, leukemoid reaction, and immune thrombocytopenia), and paraneoplastic osteoarticular syndromes (like finger clubbing) [4, 5].
Paraneoplastic neurologic syndromes (PNS) are rare in association with NC [4]. A variety of auto-antibodies have been linked to PNS, with antiYo antibodies being among the most common [6]. These antibodies are typically associated with paraneoplastic cerebellar degeneration but have been linked to other PNS as well [7]. Although antiYo antibodies are typically found in women with gynecological tumors, isolated cases have been reported in other neoplasms such as prostate cancer, lung cancer, melanoma, and pleural mesothelioma [7]. Only one prior case of an association between antiYo antibodies and head and neck carcinoma (HNC) has been reported in the literature [8].
DESCRIPTION
A 70-year-old healthy man presented to our hospital with a progressive gait disturbance. He denied weakness, sensory disturbances, bulbar or dysautonomic symptoms, as well as extrapiramidal manifestations. Physical examination revealed a moderate hypoesthesia involving light touch, vibration and pain below the knees, with positive Romberg´s sign. Hyperreflexia was noted in lower limbs, with plantar reflex being extensor in his left side. A moderate spastic-ataxic gait was observed. Biochemical, haematological and microbiological analyses were normal. A neurophysiological study showed a marked alteration in evoked somatosensorial potentials in lower limbs, with moderate decrease in evoked motor potentials in upper limbs and normal peripheral nerve conduction. A cranial-cervical MRI did not show any abnormalities at intracranial structures or cervical spinal cord, but a mild thickening of the nasopharyngeal mucosa. Cerebrospinal fluid (CSF) analyses revealed a mononuclear pleocytosis (23 cells per millilitre) with mild increase of proteins (65 mg/dL) and normal glucose (55 mg/dL). No malignant cells were detected. Both, intrathecal immunoglobulin synthesis and oligoclonal bands were detected in CSF. An extended-immunological analysis showed the existence of antiYo antibodies. With a clinical suspicion of paraneoplastic myelitis, a body CT was done revealing no significant abnormalities. Afterwards, a Fluorine-18 2-fluoro-2-deoxyglucose (F-18 FDG) positron emission tomography/computed tomography (PET/TC) showed an hypermetabolic area (9.87 SUV) at the nasopharyngeal region, whose, histological analysis was consistent with nasopharyngeal epidermoid carcinoma (Figure 1). Our patient was initially treated with high dose endovenous steroids (methylprednisolone 500mg daily for 5 days) and gammaglobulins (0.4 g/kg daily for 5 days) experimenting mild improvement of the neurological manifestations. He was then transferred to the Oncology Department, being treated with concomitant chemo-radiotherapy. Despite an adequate response of the primary tumour, there was only partial improvement in gait disorder 16 months after having finished treatment.
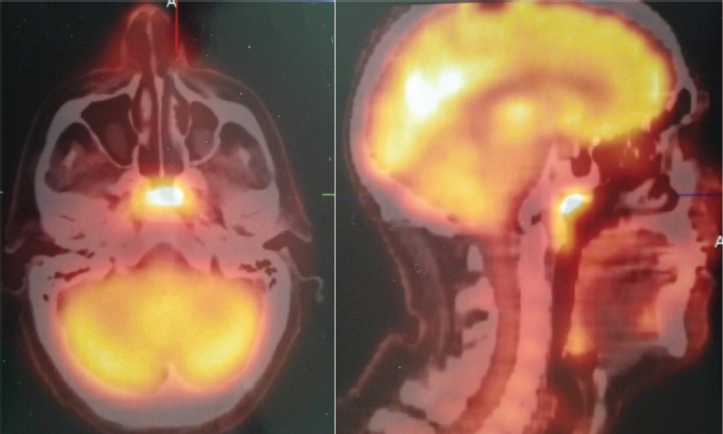
Figure 1. Fluorine-18 2-fluoro-2-deoxyglucose (F-18 FDG) positron emission tomography/computed tomography (PET/TC) shows an hypermetabolic area (9.87 SUV) at the nasopharyngeal region.
DISCUSSION
The pathogenesis of PNS is not fully understood, but immunologic factors are believed to play a significant role in many cases [9]. A commonly accepted hypothesis is that the tumor’s ectopic expression of neural antigens triggers an immune response that ultimately targets neurons expressing the shared antigen with the tumor [9].
Flanagan et al recently published a series of patients with paraneoplastic myelitis [10]. Like our case, most patients experienced a subacute onset with mild pleocytosis and elevated protein levels in the cerebrospinal fluid (CSF) [10]. Amphiphysin-immunoglobulin G was the most prevalent autoantibody in that series, detected in nearly 30 % of the patients. Anti-Yo antibodies were associated with only one case [10].
PET/CT is a valuable screening tool for evaluating patients with suspected PNS. In our case, while MRI showed mild thickening of the nasopharyngeal mucosa, the definitive diagnosis of NC was made using PET/CT (Figure 1), confirmed with flexible endoscopy and biopsy.
Treatment of PNS must be tailored to the individual. Therapy should be directed at the primary tumor, with high-dose steroids and immunoglobulins used in the acute phase. Although some patients experience complete remission of neurological symptoms, others only show mild improvement with antitumor therapy, and long-term sequelae are common despite adequate tumor control [9, 10].
CONCLUSIONS
In summary, our case highlights the link between NC and Anti-Yo antibodies. While rare, clinicians should consider the possibility of paraneoplastic aetiology when assessing patients with HNC who present with subacute neurological symptoms, after excluding more common causes.
REFERENCES
1.Ferlito A, Elsheikh MN, Manni JJ, Rinaldo A. Paraneoplastic syndromes in patients with primary head and neck cancer. Eur Arch Otorhinolaryngol 2007; 264:211–22. https://doi.org/10.1007/s00405-006-0217-5
2.Zuffa M, Kubancok J, Rusnák I, Mensatoris K, Horváth A. Early paraneoplastic syndrome in medical oncology: clinicopathological analysis of 1694 patients treated over 20 years. Neoplasma 1984; 31:231–6.
3.Morales-Angulo C, Megia LR, Rubio SA, Rivera HF, Rama J. Carcinoma of the nasopharynx in Cantabria. Acta Otorrinolaringol Esp 1999; 50:381-386.
4.Toro C, Rinaldo A, Silver C, Politi M, Ferlito A. Paraneoplastic syndromes in patients with nasopharyngeal cancer. Auris Nasus Larynx 2009; 36:513-520.
5.Maalej M, Ladgham A, Ennouri A, Ben Attia A, Cammoun M, Ellouze R. The paraneoplastic syndrome in nasopharynx cancer. 32 cases. Presse Med 1985; 14:471–4.
6.Peterson K, Rosenblum MK, Kotanides H, Posner JB. Paraneoplastic cerebellar degeneration. I. A clinical analysis of 55 anti-Yo antibody-positive patients. Neurology 1992; 42:1931-1937.
7.Chan KH, Leung SY, Cheung RT, Ho SL, Mak W. Paraneoplastic motor neuropathy and inflammatory myopathy associated with nasopharyngeal carcinoma. J Neurooncol 2007;81:93–6 inoma. J Neurol Neurosurg Psychiatry 2007; 78:775-777.
8.Bhardwaj S, Khasani S, Benasher D. et al. Paraneoplastic Cerebellar Degeneration in Nasopharyngeal Carcinoma: a Unique Association. Cerebellum, 2019; 18:1126–1129. https://doi.org/10.1007/s12311-019-01045-1
9.Darnell RB, Posner JB. Paraneoplastic syndromes involving the nervous system. N Engl J Med 2003; 349(16):1543-1554.
10. Flanagan EP, McKeon A, Lennon VA, Kearns J, Weinshenker BG, Krecke KN et al. Paraneoplastic isolated myelopathy: clinical course and neuroimaging clues. Neurology 2011; 76:2089-2095.