ADCAIJ: Advances in Distributed Computing and Artificial Intelligence Journal
Regular Issue, Vol. 13 (2024), e31939
eISSN: 2255-2863
DOI: https://doi.org/10.14201/adcaij.31939
Evaluation and Refinement of Elbow Recovery in Sports Medicine Using Smart Tracking Technologies
Sergio Alonso-Rollána, Sergio Márquez-Sáncheza,b, Albano Carrerab, Isaac M. S. Froesb, and Juan F. Blancoc
a BISITE Research Group, University of Salamanca, Calle Espejo s/n. Edificio Multiusos I+D+i, 37007 Salamanca, Spain
b Air Institute, IoT Digital Innovation Hub, 37188 Salamanca, Spain
c Department of trauma and orthopaedics surgery, Spine Unit, University Hospital of Salamanca, IBSAL, Spain
✉ sergio.alro@usal.es, smarquez@usal.es, acarrera@air-institute.com, ifroes@air-institute.com, jfblanco@usal.es
ABSTRACT
Elbow injuries, prevalent in various sports, significantly impact an athlete’s performance and career longevity. Traditional rehabilitation methods, while effective to a degree, often miss the mark in terms of precision and personalised care. This gap necessitates a shift towards more sophisticated rehabilitation strategies. This study introduces a pioneering approach in elbow rehabilitation, utilising cutting-edge wearable tracking technologies along with the telerehabilitation paradigm. The focus is on increasing the precision and efficacy of rehabilitation processes. We developed a state-of-the-art wearable device, equipped with sophisticated sensors, to accurately track elbow joint movements, including position, rotation, and flexion, in real-time. The device provides detailed data, allowing for nuanced diagnosis and effective monitoring during rehabilitation phases. This data is integrated into a specialised application, enabling comprehensive data analysis and the formulation of personalised rehabilitation plans with real-time feedback. The device demonstrated a notable improvement in the precision of monitoring and effectiveness of rehabilitation strategies, allowing the measurement of the range of motion (RoM) within an error of ±3 degrees. A comparative analysis with traditional methods revealed significant advancements in accuracy, adherence to prescribed rehabilitation regimens, and overall speed of recovery.
KEYWORDS
elbow rehabilitation; wearable technology; sports medicine; telerehabilitation; athlete recovery
1. Introduction
Elbow injuries in athletes, particularly those involved in overhead and racket sports, represent a significant challenge in sports medicine. These injuries, ranging from acute conditions such as fractures to chronic issues such as tendinopathy, have profound implications on an athlete’s performance and career longevity. Traditional rehabilitation approaches, while beneficial, often fall short in providing the personalised monitoring and real-time data analysis necessary for optimal recovery. This gap is particularly evident in the context of athlete care, where the need for precise, real-time monitoring and tailored rehabilitation strategies is critical for effective treatment and swift return to sport. This paper introduces an innovative approach to elbow rehabilitation, leveraging recent advancements in wearable technology to improve recovery outcomes. This approach not only enhances the precision and personalisation of rehabilitation but also aligns with the evolving landscape of data-driven, patient-centred healthcare. The objectives of this paper are to (i) demonstrate the effectiveness of wearable technology in the real-time monitoring and analysis of elbow joint movements, (ii) illustrate the integration of this technology with a tele-rehabilitation platform for personalised care, and (iii) evaluate the impact of this integrated system on rehabilitation outcomes compared to traditional methods.
Central to this approach is the development of a telerehabilitation and personalised patient monitoring software system, which is complemented by a wearable device, designed specifically for the elbow. The wearable, which has been designed as a cost-effective tool, integrates advanced sensors that allow to take objective and accurate measurements. The telerehabilitation software is a distributed system consisting of a mobile application, which the user installs on their phone, and of a web platform that facilitates monitoring, remote follow-up and personalised treatment for athletes.
The platform provides healthcare staff with solid data on the evolution and recovery trends of the people under their care. They are able to visualise advanced graphs on joint rotation and flexion, and the evolution of the patient’s mobility. This technology allows for a more comprehensive diagnosis and helps in the monitoring of the athlete’s condition throughout their rehabilitation. The system, through the detailed analysis of the data, facilitates personalised rehabilitation strategies, and given that it is combined with the wearable.
The effectiveness of wearable technology in rehabilitation is supported by a range of studies. First of all, the review presented by Faisal et al. presented a series of methods for the continuous monitoring of the joints in the human body, and wearable devices were marked as a significant tool for this purpose (Faisal et al., 2019). The thesis of Hristov was on the intersection of wearable technology and health monitoring (Hristov, 2023). Rodgers et al. explored the evolving role of wearables in sports medicine (Rodgers et al., 2019). Zadeh and colleagues investigated the use of wearables for forecasting and preventing sports injuries (Zadeh et al., 2021). Seçkin et al. provided a comprehensive overview of the growing significance of wearables in enhancing sports performance and rehabilitation processes (Seçkin et al., 2023). Additionally, several studies demonstrated the suitability and effectiveness of the telerehabilitation processes compared with the traditional on-site clinical rehabilitation processes (Nuevo et al., 2021; Seron et al., 2021) or (Höher et al., 2023).
Recognising the dynamic nature of sports and the specific physiological needs of athletes, this study advocates for a more adaptive and responsive approach to rehabilitation. Wearable technology, with its capability for real-time data collection and analysis, offers an unprecedented level of insight into an athlete’s recovery process. The ability of these devices to provide sensor-based feedback means that rehabilitation programs are tailored to the needs of individual athletes, thereby enhancing treatment effectiveness. In addition to collecting and analysing real-time data, the repeatability that can be achieved in the measurements is noteworthy (Fennema et al., 2019).
Moreover, the methodologies developed for athlete rehabilitation in this study, have broader healthcare implications. They can be adapted for managing chronic musculoskeletal conditions, reflecting the convergence of sports medicine, technology, and general healthcare. This points to a future where personalised, data-driven care is the standard, significantly improving patient outcomes across different groups.
This article is structured as follows: Section 2 provides a comprehensive review of current technologies and methodologies in elbow rehabilitation, along with a critical analysis of related literature. Section 3 describes the architecture and design of the developed elbow rehabilitation system. Section 4 presents the results obtained from the system’s implementation and compares them with existing solutions. Finally, Section 5 summarises the study’s findings and discusses potential future advancements in the field of sports medicine and rehabilitation.
2. State of the art
In the rapidly evolving field of sports medicine, the integration of technology into rehabilitation practices has marked a significant shift in treatment paradigms. This state-of-the-art section delves into the multifaceted approach to managing elbow injuries in athletes, an area that has seen considerable advancements thanks to the advent of wearable technology. By examining the nature and impact of common elbow injuries, along with the challenges faced in traditional rehabilitation methods, this section aims to establish a foundation for understanding the pivotal role of technology in revolutionising athlete care. The focus on elbow injuries is particularly relevant given their frequency and potential impact on an athlete’s career. This exploration is not only crucial for healthcare professionals and athletes but also offers insights to researchers and technologists who strive to advance the innovation in this field.
2.1. Background on Elbow Injuries
Elbow injuries among athletes, particularly those engaging in sports involving overhead arm motions, are becoming increasingly common. Fractures of the elbow are usually very complex joint injuries that often require surgical treatment. The elbow joint allows flexion-extension and pronation mobility that places the hand at different points in space. Three joints converge at the elbow, the one comprising the ulnotrochlear, the radiocapitellar and finally the proximal radioulnar joint. This elbow joint tends to stiffness after fractures or ligament injuries which causes a very important functional impairment. For this reason, starting rehabilitation in a very early and controlled manner is necessary in order to restore the range of motion while not compromising the stability of the osteosynthesis or ligament repair performed (Ozel and Demircay, 2016).
Among the injuries that most frequently cause post-surgical stiffness are distal humeral fractures and the so-called terrible triad injuries. These injuries are often aggravated by varying degrees of instability. Dislocation of the elbow is a frequent injury, as they are injuries affecting to the ligaments that stabilize the joint to allow its properly function. There exists a consensus among authors in pointing out how these injuries are frequently complicated, especially by the development of stiffness and loss of elbow mobility. Thus, treatment of the injuries should aim at stabilization, but if immobilization is prolonged, stiffness is the norm. For this reason, an early and monitored rehabilitation program seems to be a very appropriate treatment strategy (Fusaro et al., 2014; Schuberg et al., 2021).
Elbow injuries are predominantly chronic; they are overuse injuries resulting from repetitive intrinsic or extrinsic overload. These conditions result from repetitive valgus stress or axial compression, leading to a range of complications, including chondromalacia, loose bodies in joint compartments, ulnar collateral ligament injury, and myotendinous injury to the flexor-pronator muscle group. The severity and chronic nature of these injuries can significantly affect an athlete’s performance, potentially leading to interruptions in their career and deterioration in their performance levels. Effective management and treatment of these injuries are crucial to prevent long-term impact on athletes’ careers (Kliethermes et al., 2020).
Athletes are subject to both traumatic and repetitive stress injuries at the elbow joint, requiring systematic and progressive rehabilitation programs. These programs aim to restore full motion, muscular strength, endurance, and neuromuscular control in the affected elbow. However, traditional rehabilitation approaches often face challenges such as the lack of personalisation and inadequate monitoring, which are essential for the complete restoration of elbow function and enable athletes to return to their prior level of function. Multi-phased rehabilitation programs are thus crucial in avoiding overstressing healing tissues and ensuring a full recovery (Johnston and Dijkers, 2012).
2.2. Advancements in Wearable Technology
The advancements in wearable technology, particularly in the healthcare and sports medicine sectors, have paved the way for innovative approaches in athlete rehabilitation and performance enhancement. This subsection, «Advancements in Wearable Technology», explores the evolution, incorporation in sports medicine, and benefits of wearable technology over traditional methods.
The inception of wearable technology in healthcare can be traced back to the development of biosensors in controlled lab settings. One of the first notable uses was by Leland C. Clark, known as the «father of biosensors», who in 1956 employed electrodes for blood oxygen level detection during cardiovascular surgeries. This initial application paved the way for the commercialisation of glucose analysers in 1975, based on Clark’s electrochemical biosensor. With the miniaturisation of electronics and advancements in material sciences, integrated Healthcare Wearable Devices (HWDs) emerged, featuring biocompatible flexible materials such as polyethylene naphthalate, polyethylene terephthalate (PET), Ecoflex, and Polydimethylsiloxane (PDMS) for enhanced comfort and compliance. These materials’ flexibility and stretchability are well-suited for HWDs, making them suitable for long-term, uninterrupted data acquisition (Guk et al., 2019).
Wearable technology has significantly transitioned into sports medicine, becoming more accessible to athletes and teams. Technological advances have enabled the monitoring of functional movements, workloads, and biometric markers to optimise performance and minimise injury risks. Wearable performance devices in sports medicine include a variety of sensors such as pedometers, accelerometers/gyroscopes, GPS devices, heart rate monitors, sleep monitors, and temperature sensors. These devices are instrumental in providing real-time physiologic and movement parameters during training and competitive sports, aiding in designing sports-specific training programs and injury prevention strategies (Li et al., 2016).
Wearable devices in healthcare, including those used in sports medicine, have shown significant benefits over traditional methods. These devices enable continuous and real-time monitoring, which is essential for patients with chronic illnesses such as cardiovascular diseases, diabetes, and neurological disorders. Wearable sensors provide a deeper understanding of the changes in the human body, aiding in disease prevention and treatment. Their non-invasive nature simplifies therapeutic procedures and reduces infection risks associated with invasive monitoring. This real-time data collection and analysis capability of wearable devices offer numerous advantages in personalised healthcare, enhancing their utility towards tailored treatment and rehabilitation strategies (Rigamonti et al., 2020).
2.3. Wearable Technology in Injury Diagnosis and Rehabilitation
The utilisation of wearable technology in sports rehabilitation, particularly for injury diagnosis and recovery monitoring, has been transformative. These technologies enable the continuous and real-time tracking of various physiological and biomechanical parameters. For example, Del Din et al. utilised wearable sensors combined with machine learning algorithms to estimate Fugl-Meyer clinical scores in stroke survivors, demonstrating the potential for similar applications in sports rehabilitation, particularly for elbow injuries (Del Din et al., 2011). This real-time monitoring is crucial for dynamic assessments, allowing for immediate adjustments to rehabilitation strategies based on the athlete’s progress and recovery trajectory.
Personalisation in rehabilitation is increasingly important, given that clinical studies often report satisfactory motor gains only in a portion of participants. Wearable technology offers a solution to this challenge by enabling the development of patient-specific interventions. The data collected using wearable sensors, processed through machine learning algorithms, allow clinicians to tailor rehabilitation programs to individual needs. This approach is supported by the research of Morris et al. who utilised the Wolf Motor Function Test to assess upper extremity function after a stroke, demonstrating the potential for wearable technology in creating customised rehabilitation plans for sports-related elbow injuries (Morris et al., 2001).
Recent advancements in wearable technology for rehabilitation have been depicted in various studies and research projects. For instance, the methodology presented by Preatoni et al. emphasised the feasibility of using wearable sensors unobtrusively to record data relevant to the assessment of upper-limb motor function. This data, processed using machine learning algorithms, helps estimate clinical scores across different domains, enabling the continuous assessment of clinical outcomes throughout the intervention period (Preatoni et al., 2022).
Another significant development in wearable technology for rehabilitation was highlighted in a report by Medical Tech Outlook. Current wearable technologies have been adapted to address follow-up and activity issues post-surgery. For instance, the use of IoT enables surgeons to remotely track patients’ activities and monitor wound healing. Additionally, the combination of biometrics, sensors, and algorithms for motion analytics allows for a more nuanced analysis of a patient’s recovery, facilitating enhanced patient management. This technology has also been integrated into sports biomechanics to develop tailor-made training programs and adjust training devices, further enhancing the personalisation aspect of rehabilitation (Meijer et al., 2018).
Recent advancements in wearable technology have significantly impacted the field of elbow rehabilitation. Brookshaw et al. (2020) introduced a novel wearable device specifically designed for measuring elbow strength, showcasing its reliability and validity. This development is crucial for accurately assessing the progress of rehabilitation and ensuring targeted exercises are effectively enhancing elbow strength. Rahman et al. (2021) explored the use of wearable sensors for classifying electromyographic signal patterns related to changes in the elbow joint angle. Their work demonstrates the potential of wearable technology in providing detailed insights into muscle activity and movement patterns, which is essential for tailoring rehabilitation exercises to the specific needs of patients. Kim et al. (2020) conducted an analysis using machine learning-based assessments for elbow spasticity with inertial sensors. Their findings highlight the role of advanced algorithms in understanding and quantifying spasticity levels, offering a more nuanced approach to managing and rehabilitating elbow spasticity.
Rose et al. (2017) utilised wearable inertial sensors for the quantitative assessment of shoulder and elbow kinematics in a cadaveric knee arthroscopy model. This study underscores the precision and applicability of wearables in simulating real-world conditions and improving surgical techniques and rehabilitation protocols. Lastly, McGibbon et al. (2013) focused on the clinical evaluation of elbow spasticity during passive stretch-reflex using a wearable sensor system. Their research provides valuable data on the natural responses of the elbow to passive movements, aiding in the development of rehabilitation strategies that accommodate the unique physiological reactions of patients.
2.4. Implementation Challenges and Considerations
While wearable technology has immense potential in sports rehabilitation, several technical challenges must be addressed. A primary concern is the development of comprehensive applications («killer apps») that can fully harness the capabilities of wearable devices. Current applications are mostly limited to basic fitness tracking features, such as heart rate monitoring and calorie intake. Without a variety of robust apps that meet diverse consumer needs, the widespread adoption and utility of wearable devices in sports rehabilitation may be limited (Cardinale and Varley, 2017). Additionally, power management, technological dependence, managing wireless and personal area networks (PAN), and ensuring security from potential hackers are significant challenges. These issues require advancements in software architecture, particularly for small-screen interfaces and robust security measures to protect the data stored on the device (Seshadri et al., 2016).
The adoption of wearable technology in the athletic community has been progressive, with professional sports leagues such as the NFL incorporating these devices to track various metrics. Wearables are used to monitor an athlete’s performance, including aspects such as speed, completion rates, and other relevant data points. This technology is not limited to professional levels but extends to colleges and high schools. However, the adoption rate varies, and the extent to which athletes and coaching staff embrace this technology can depend on several factors, including awareness, perceived benefits, and the availability of technology (Kastoriano and Halkias, 2020).
In the development of our experimental design for elbow rehabilitation, we meticulously analysed the current state of the art in Wireless Sensor Networks (WSN) within the rehabilitation domain. Our investigation was guided by seminal works that underscore the pivotal role of WSN in enhancing rehabilitation processes through innovative monitoring and intervention strategies. Hadjidj et al. (2013) provide a foundational perspective on the utilisation of WSN in rehabilitation, highlighting both the challenges and opportunities that come with integrating these technologies into patient care. Their insights into the dynamic capabilities of WSN for real-time patient monitoring and data analysis form the backbone of our experimental approach, aiming to leverage these technologies to improve outcomes in elbow rehabilitation. Building on this foundation, the work of Idoudi et al. (2018) showcases a sophisticated application of wireless visual sensor networks for the accurate localization and tracking of patients during rehabilitation tasks. This approach aligns with our objective to precisely monitor patient movements and adjust rehabilitation protocols based on real-time feedback, ensuring a personalised and effective rehabilitation process. Moreover, Ali et al. (2018) extend the discussion by reviewing various applications of WSN in monitoring rehabilitation efforts across different settings. Their comprehensive analysis not only validates the versatility of WSN technologies but also informs the scalability and adaptability of our experimental design, accommodating diverse rehabilitation needs and settings.
Through the integration of these pivotal studies, our experimental design aims to push the boundaries of conventional rehabilitation practices. By harnessing the advanced monitoring capabilities of WSN, we are setting new standards for personalized care in elbow rehabilitation, ensuring that our methodologies are both innovative and grounded in the latest research advancements. This state-of-the-art review forms the foundation of our approach, positioning our work at the forefront of technological integration in rehabilitation sciences.
The use of wearable technology in sports raises significant ethical and privacy concerns. Questions arise over data ownership, particularly in professional leagues where teams may use data in contract negotiations, but athletes might not have full access to their information. This debate extends to how and where the data is stored, used, disclosed, who has access, and what safeguards are in place to protect it. Furthermore, wearable devices can collect sensitive personal information relating to an athlete’s identity, location, or health status. Such data collection poses privacy and security risks, and compliance with international, federal, and state data protection laws becomes crucial. Sports and athletic organisations need to be mindful of these risks and regulatory issues when developing wearable device programs (Segura Anaya et al., 2018).
2.5. Future Directions and Potential
The future of wearable technology in sports medicine is poised for groundbreaking advancements. Upcoming technologies are expected to bring about significant improvements in athlete monitoring, injury prevention, and rehabilitation. Innovations may include advancements in sensor accuracy, miniaturisation, and integration with artificial intelligence (AI) and machine learning (ML) algorithms. These technologies could offer more nuanced data analysis, enabling more precise diagnostics and targeted interventions. For instance, the integration of AI and ML in wearable devices could facilitate the development of predictive models that identify injury risks before they occur, allowing for timely preventative measures (Greco et al., 2023).
The methodologies and technologies developed for sports rehabilitation have immense potential to be applied in broader healthcare settings. The ability of wearable technology to provide real-time health monitoring and personalised data analysis can be crucial in managing chronic diseases, post-operative recovery, and elderly care (Ryan et al., 2014). By leveraging the lessons learned from sports medicine, healthcare providers can develop more effective treatment plans and intervention strategies. This could lead to enhanced patient outcomes across different medical fields, including cardiology, neurology, and orthopaedics, where continuous monitoring and personalised treatment plans are essential.
Looking ahead, the field of sports medicine is likely to witness significant changes, driven largely by advancements in wearable technology. Future trends may include the development of more sophisticated sensors capable of tracking a wider range of physiological and biomechanical parameters. There is also a potential for increased integration of wearable technology with other digital health platforms, creating a more interconnected and comprehensive approach to athlete health management. Furthermore, as data analytics becomes more advanced, sports medicine professionals could gain deeper insights into injury prevention, training optimisation, and recovery processes. This evolution is likely to not only benefit elite athletes but also recreational sports enthusiasts, contributing to overall health and fitness improvements (Zadeh et al., 2021).
2.6. Comparative Analysis and Novelty of the System
In the rapidly evolving field of sports medicine and rehabilitation, wearable technology has emerged as a transformation tool for injury diagnosis and recovery monitoring. The integration of such technology offers continuous, real-time tracking of physiological and biomechanical parameters, significantly enhancing the personalisation and effectiveness of rehabilitation programs. Our system, leveraging state-of-the-art wearable sensors and tele-rehabilitation platforms, represents a significant advancement in this area. Not only does it allow for precise tracking of elbow joint movements but also enables the formulation of personalized rehabilitation plans through comprehensive data analysis and real-time feedback. This approach addresses the critical need for more customized and responsive rehabilitation strategies, which is often highlighted as a limitation in existing studies.
Below, we present a comparative analysis of our work with related studies in the field, highlighting the unique contributions and advancements our system offers. Table 1 provides an insightful comparison between our system and existing studies focused on wearable technology’s role in injury diagnosis and rehabilitation. This comparison underscores our system’s superior ability to offer real-time feedback and personalized rehabilitation plans, setting a new standard in the precision and customization of care for elbow injuries.
Table 1. Comparative table of related works wearable technology in injury diagnosis and rehabilitation
Reference |
Considerations |
Focus: Wearable sensors for stroke rehabilitation. Advantages: Utilises machine learning for clinical score estimation. Limitations: Focused on stroke, not specifically on elbow injuries. Comparison with our work: Our work extends the application to elbow rehabilitation with enhanced precision and real-time feedback. |
|
Focus: Assessing upper extremity function post-stroke. Advantages: Demonstrates potential for customized rehabilitation plans. Limitations: Limited to stroke rehabilitation. Comparison with our work: We offer a broader application with focus on sports-related elbow injuries and personalized care. |
|
Focus: Wearable sensors for upper-limb motor function. Advantages: Feasibility of unobtrusive data recording. Limitations: Lacks of integration with tele-rehabilitation platforms. Comparison with our work: Our system integrates data with a tele-rehabilitation platform for. |
|
Focus: IoT and wearables in post-surgery care. Advantages: Enhanced patient management through technology. Limitations: It is not specifically addressing elbow rehabilitation. Comparison with our work: Our system specifically focuses on elbow rehabilitation, offering tailored recovery monitoring. |
Subsequently, Table 2 delves into a broader spectrum of research, including our work’s comparative analysis against recent significant advancements in elbow rehabilitation. This table highlights our system’s unique contribution in extending the application of wearable technologies to offer a more comprehensive and nuanced approach to rehabilitation, which is not only focused on enhanced precision and real-time feedback but also on integrating these technologies with tele-rehabilitation platforms for a holistic care model.
This leap in technological application is delineated through our comparative analysis, represented in Table 1 and Table 2, which places our work in direct contrast with prior studies. By leveraging advanced sensors and integrating comprehensive data analysis with real-time feedback mechanisms, our system sets a new benchmark in customized care, responding dynamically to the evolving needs of patients. It is through this perspective of innovation, precision, and personalisation that our system stands as a pioneering solution in the domain of sports medicine and rehabilitation, paving the way for future advancements in patient care.
Table 2. Comparative table of related works on elbow rehabilitation
Reference |
Considerations |
Focus: Novel wearable device for measuring elbow strength. Advantages: High reliability and validity. Limitations: Focused primarily on strength measurement, not comprehensive motion analysis. Comparison with our work: Our system offers a broader range of motion analysis, enhancing rehabilitation with precise tracking and feedback. |
|
Focus: Classification of EMG signals by elbow joint angle changes. Advantages: Innovative use of wearable sensors for EMG signal analysis. Limitations: Limited to signal pattern classification, not direct rehabilitation application. Comparison with our work: Our work integrates direct rehabilitation applications, offering real-time feedback and personalized plans. |
|
Focus: Elbow spasticity assessment using inertial sensors and machine learning. Advantages: Applies machine learning for assessing spasticity. Limitations: Focused on spasticity, not on a broader range of rehabilitation needs. Comparison with our work: We encompass a wider spectrum of elbow rehabilitation needs, employing machine learning for personalised treatment strategies. |
|
Focus: Quantitative assessment of shoulder and elbow kinematics. Advantages: Precise kinematic assessment with wearable sensors. Limitations: Limited to human models, not applications with patients. Comparison with our work: Our system is designed for live patient applications, facilitating real-time monitoring and adjustment of rehabilitation plans. |
|
Focus: Clinical evaluation of elbow spasticity using wearable sensors. Advantages: Effective in clinical evaluation of spasticity. Limitations: Focused on passive stretch-reflex, not active rehabilitation. Comparison with our work: Our platform supports both passive and active rehabilitation strategies, enhancing patient engagement and recovery outcomes. |
3. System Architecture and Design
The architecture of the elbow rehabilitation monitoring system is designed to meet the requirements of a customisable, wearable-based, patient-centric telemedicine system. The proposed architecture must achieve several functional requirements at the level of the IoT wearable, the mobile application and the web platform, Table 3, Table 4 and Table 5 summarise all these requirements.
Table 3. Wearable device (IoT) level functional requirements
Level |
Functional Requirement |
Wearable |
Elbow Range of Motion (ROM) measurement. The wearable device must be able to detect the joint angle from the straight arm reference, 0 degrees; it should be able to detect certain level of hyper extension, -10 degrees, and flexion measurements up to the user’s maximum angle, 150 degrees (Oosterwijk et al., 2018). |
Wearable |
Measurement Accuracy. The device must collect clinically useful measurements; thus, the obtained data should be comparable to that collected with the goniometer. |
Wearable |
Ease of Use and Accessibility. The device must be usable by any user, so that useful measurements should be taken by means of few interactions with the device or the app. These conditions ensure that the device is accessible to as many users as possible. |
Wearable |
Battery. The operation must be portable; therefore, batteries must be used as a power source. |
Wearable |
Comfort and Ergonomics. The device should be comfortable so as not to cause problems for the patient, such as discomfort or chafing. In addition, the system should be lightweight to avoid overloading on the arm, comfortable for the user and adaptable to different physiognomies. |
Wearable |
Removable. To ensure that the cloth where the device is placed is washable, the device must be removable. |
Wearable |
Bluetooth Communication. The connection between the wearable and the mobile application should be wireless by Bluetooth Low Energy (BLE). |
Table 4. Mobile application (App) level functional requirements
Level |
Functional Requirement |
App |
Data Collection and Storage. The developed mobile application must be able to collect the data transmitted by the wearable device via BLE. The received data must be stored until it is uploaded to the Cloud via an Internet connection. |
App |
Authentication. The application must be accessible to users through a username and password; the system must secure access and allow each patient to have a personal and non-transferable profile. Data associated with the patient must be classified internally. |
App |
Forms. The application should allow clinical staff to provide follow-up care to patients in order to assess their progress; therefore, patients should be able to complete follow-up forms via the application. These forms must be customised for each lesion and for each user. |
App |
Collected Data. The patient is able to consult the data and statistics on the evolution of their injury via the mobile application. Additionally, challenges are included as a motivational strategy for the patient’s rehabilitation. |
App |
Gateway. The mobile application must serve as a gateway between the wearable device and the cloud. Therefore, Wi-Fi or cellular connectivity to send the collected data to the server is a must. |
To achieve correct functionality, the system must at least meet all the functional requirements presented in Table 3, Table 4 and Table 5. In addition, with regard to the technical aspects, the following are the key points that have been used as a reference so that the system is stable and, in addition, meets the expectations: (i) System availability, the data must be available at any time, along with the rest of the functionalities listed in Table 3, Table 4 and Table 5, so that both patients and clinical staff can access them. (ii) System performance, the user waiting times should not be excessive, and data loading should be performed with sufficiently short server response times. (iii) Scalability of the system, optimal performance must be guaranteed even though the number of users may grow. (iv) Security, data exchanges must be carried out with a secure data protocol to ensure that information is not exposed, and data stored in the database must be properly secured. (v) Privacy, data confidentiality must be guaranteed, only the users that have permissions should be able to access the patients’ clinical and personal information.
Table 5. Web platform level functional requirements
Level |
Functional Requirement |
Web |
Patient Management. The platform must allow clinical staff to keep track of their assigned patients while respecting their data confidentiality. Thus, the processes of registering, de-registering and modifying their assigned patients should be allowed. This point also includes access to the collected data, forms and the customisation of these forms. |
Web |
Clinical Staff Management. The platform should allow an administrator to manage the clinical staff that has access. In addition, administrator users do not need to have access to patient data. |
Web |
Interface. Users must have access to all available options according to their role, the displayed information must be neat and tidy, and the look and feel must be user-friendly. This would facilitate access to the platform and its integration in the clinical environment for staff who are less familiar with web environments and have less IT knowledge. |
Web |
Cloud Storage. Both the collected data and the patient forms must be stored securely and encrypted in the cloud, and they should be accessible by both the clinical specialists and the patient themselves. |
Web |
Telemedicine. The platform should serve as a telemedicine tool, remotely monitoring patient recovery, based on objective data collected by the wearable device. To allow for more comprehensive monitoring in the event of complications, alerts should be available for set up. |
3.1. Architecture Definition
The architecture has been developed based on a layered pattern, that provides a level of abstraction in which each layer provides a service to the layer above it. In this particular case, the Edge layer is in charge of collecting measurements and, thus, providing data to the Cloud layer. Figure 1 shows a diagram of the complete architecture. The layers, which are represented in different colours, integrate the devices and parts presented in the requirements (Table 3, Table 4 and Table 5) and contribute to the correct functionality of the system. Fundamentally, the architecture is divided into two main layers, the cloud and the edge, each of which plays a vital role so as to achieve the presented functionality. The cloud layer, which is aimed at the administrator and clinical staff, has been divided into three different parts in order to meet the requirements. On the other hand, the edge layer, whose usability is focused on patients, enables interaction with the wearable device through a mobile application. Table 6 summarises the information regarding each of the parts included in the system.

Figure 1. Architecture of the developed system
Table 6. Parts of the system and the layers to which they belong
Level |
Part |
Description |
Cloud |
Front-end |
The visual interface, which is offered via the web, allows the user to interact with the system. The front-end is implemented in Vue.js. |
Cloud |
Back-end |
The back-end implements all the logic necessary for the proper functioning of the system. This part is responsible for managing access to data, ensuring privilege access, and implementing the functionality provided by the front-end. |
Cloud |
Database |
The persistent storage is provided by a database using the MySQL management system. To filter unauthorised access and to apply the defined level of privilege, the database is not directly accessible, the access is managed by the back-end of the system. |
Edge |
IoT Wearable |
The IoT wearable device provides the functionality to monitor the patient’s elbow flexion angle (ROM), tracking the patient’s recovery progress. This device sends the data via BLE to the mobile application. |
Edge |
Mobile Application |
The patient centred mobile app, which is implemented on Android, collects IoT device data. In addition, the app can collect data from customisable forms about the patient’s progress. The collected data is sent to the cloud, where it is stored, via a secure REST API. |
The cloud layer hosts the telerehabilitation platform, consisting in three elements. First of all, the database provides the persistent storage functionality of the system implemented through the MySQL database management system. This element is not directly accessible, its access is managed by the back-end of the system, which allows filtering unauthorised access and applying the privilege scale defined for the system. Secondly, offered via the web, the front-end is the visual interface, which allows the user to interact with the system. It is implemented in Vue.js and implements the roles of «Administrator» and «Healthcare professional» (these roles will be explained on section 3.2. In third place, the back-end implements all the logic necessary for the proper functioning of the system. This part is responsible for managing access to data, ensuring the scale of privileges, and implementing the functionality offered by the front-end. Although the user, in this case, the healthcare professionals interact with the system through the front-end, it must be assumed that the web platform is made up of the three elements mentioned above, as one without the others would be useless.
The edge layer implements the data collection functionality to serve the telemedicine platform hosted in the Cloud. The edge layer has two main elements. The first one is the wearable IoT device, which provides the functionality to monitor the elbow flexion angle, allowing the tracking of the patient’s recovery progress. This element sends the data via Bluetooth Low Energy (BLE) to the mobile application. Then, the mobile app is responsible for receiving data from the IoT device, and additionally, it collects data from customisable forms regarding the patient’s state and progress. The app is also in charge of combining the wearable data with the information from the forms. All collected data is sent to the cloud where it could be processed and stored permanently. The application is implemented natively in Android, using Kotlin as the language. It communicates with the Cloud using a REST API.
3.2. User Roles and Interactions
In the system, three distinct user roles have been identified, each with specific interactions and privileges within the system. Each role is carefully designed to ensure that the system operates efficiently and securely, catering to the specific needs of the patients and responsibilities of the healthcare professionals and administrators. Figure 2 illustrates the different roles, showing the type of components with which each of them interacts. In addition, the dependency between each of the roles is shown.
• Patient User: This role is assumed by patients utilising the system for their rehabilitation. These users interact with the system primarily through the IoT wearable device and the mobile application. In terms of access, patients have the lowest level of privileges; this access is limited to viewing and accessing data about their own treatment. Importantly, patients do not have the ability to create accounts on their own; instead, they are registered in the system by their assigned healthcare professional.
• Healthcare Professional User or Clinical Staff: These users are responsible for the rehabilitation and recovery of patients. Their role involves managing patient registrations, modifications, and monitoring their progress through the web platform. The clinical staff have access to the data of all patients under their care, and they can view the latest data that has been collected, responses to control forms, and have the ability to assign or modify these forms as needed. Their interaction with the system is through the web platform.
• Administrator User: The role with the highest-level privilege hierarchy in the system; the administrator role involves overseeing and managing the clinical staff who have access to the platform, and they do not have access to any patient information nor to the collected data. Similarly to the healthcare professionals, administrators interact solely with the web platform and do not use the mobile application.
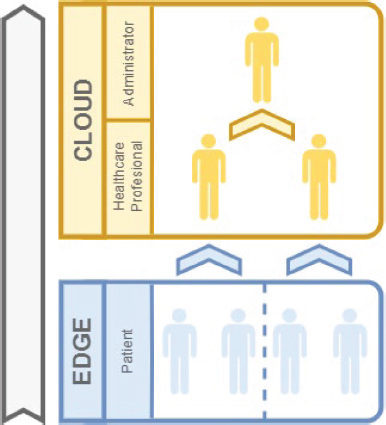
Figure 2. User roles diagram related to the different parts of processing
3.3. Web Platform
The web platform has been designed to specifically cater to the needs of administrators and healthcare professionals. The platform structure adapts to the specific roles of these users, with functionalities tailored to enhance efficiency and management in rehabilitation processes. A screenshot of the platform is shown on Figure 3. As it has been previously presented in this section, there are three different users in the system, each of them has access to certain parts of the platform, taking into account the role they play within the system.
Administrator User
As previously explained, administrators are the superuser of the system; after logging in they are shown a dashboard which allows them to manage the system’s operations in different areas:
• Doctors: This section allows administrators to manage doctor profiles, including viewing, editing, and deleting options. It also provides a comprehensive view of each doctor’s patient list.
• Alerts: Administrators can create, modify, and delete alerts within the system, managing critical notifications relevant to patient care.
• Advice and Challenges: This area enables the addition and management of rehabilitation advice and challenges, enhancing patient engagement in the recovery process.
• Questionnaires: The platform allows for the creation and editing of questionnaires, setting their frequency, and determining the required responses, aiding in patient assessment. The questionnaires are completely adaptable, and they allow for the use of different type of questions, such as multiple answer, picture attachment for monitoring wounds or visual analog scale for subjective information reporting, among others.
• Pathologies: Administrators can manage a list of pathologies, adding and deleting them from the system, as necessary.
Additionally, administrators do not have access to patient information or data, their role is just to ensure data integrity and security. Thus, the administrator may only get information about the number of patients assigned to a doctor or if the patients are using the platform, but in an anonymous way for monitoring purposes. In what regards patients, administrators do not have data editing capabilities; all the clinical information is protected.

Figure 3. Platform home screen for the administrator role. On the left side, there is a menu that is always accessible, in the central part there are shortcuts to each section with a brief description (in the Spanish language)
Healthcare Professional User
The doctors or healthcare professionals have a similar dashboard, but some areas are not accessible, and each user is allowed to manage their own patients. Thus, the focus of the dashboard is on the patient follow-up and recovery process.
• Patient Management: Doctors have access to detailed patient profiles, including session statistics and personal information, and can manage patient registrations and monitor their progress.
• Session Review: This feature allows healthcare professionals to review and analyse patient sessions and rehabilitation progress through graphical data representations.
• Questionnaire Access: Doctors have the ability to view and assign questionnaires to patients, though with limited functionalities compared to administrators.
Healthcare professionals primarily interact with the platform via the web interface, focusing on patient care and progress monitoring.
Patient User
Patients engage with the system exclusively through the mobile application and do not have access to the web platform. This design ensures ease of use and accessibility, making the rehabilitation process more patient-friendly.
3.4. Scalability of the Whole System
The proposed architecture is based on a distributed system. As they are defined, the distributed systems are more scalable than a traditional monolithic system. These architectures allow replicating each element of the system individually, as long as the communication interfaces designed and defined in previous subsection are adhered to. Figure 3 illustrates a graph of the system’s scalability through the replication of the aforementioned and explained components. Each component of the system can be horizontally replicated without affecting other elements of the system. This form of independent scalability facilitates the expansion of the system in the future. Therefore, expansion or reduction of any nodes in the architecture is permitted.
Regarding the edge environment, it is possible to replicate the IoT device or the mobile application, ensuring there is one device and one version of the application for each patient. Furthermore, it would be possible to duplicate the edge layer, creating different independent edge environments that connect to the same cloud layer.
Concerning the cloud layer, in the same way and following a consistency paradigm between layers, a scaling system is proposed in which the server hosting the cloud could be completely replicated, without replicating the elements independently. However, this is just a simplified approach to the system’s scalability; despite this fact, scale individual components of the cloud due to their micro-services nature would still be possible. In a micro-service based architecture, where each module handles a specific and limited functionality, each system function is executed through independent modules; following this approach each component contributes running a part of the overall functionality, and the sum of all these components constitutes the complete system.
3.5. Data Security
Taking into account the scientific literature centred on security in IoT systems, Huanan et al (2021) analyses this matter on exploitation environments, which have vulnerabilities different from traditional ones due to their distributed structure. After the relevant study, the need to pay attention to security at all levels of the network is established: Confidentiality, key management, data integrity, data freshness, auditability, non-repudiation, and access authentication. The following points have been secured in this system:
• Confidentiality: In order to prevent any external user to be able to decode the data collected from or about the patient, data is sent encrypted by BLE between the device and the gateway. On the upper layers, data is sent using an API based on HTTPS secured protocol which guarantees the information protection.
• Key management: The platform allows updating of key access.
• Data integrity: Data is stored in a remotely inaccessible database. This database can only be accessed through REST API that controls whether requests, both read and write, are allowed for the user.
• Data freshness: The device is linked to the mobile application, and data from any unauthorized device is not accepted. In this way, false data introduction into the communication flow by any malicious individuals is prevented.
• Access authentication: The system only allows access to registered users. Additionally, the implemented user role system ensures that each user only have access to data permitted according to his/her role.
3.6. Hardware and Mechanical Design
By definition, all telemedicine or telerehabilitation systems need an interface between the patient and the monitoring platform. In the present development, the interface is a wearable device for the arm. Thanks to this device, the remote monitoring of the patient is achieved along with patient interaction and clinical follow up. The aforementioned device records the measurements of rotation and flexion from the elbow joint. Thus, to record the metrics for the assessment of the clinical recovery, the wearable must be worn by the user. After that, all the collected data are processed by the healthcare professional through the telerehabilitation platform along with the answers received to customised forms.
To provide the platform with the data regarding the range of movements of the patient’s joint, the hardware of the wearable device has been designed and developed. The purpose of this device is to monitor the angle formed by the elbow joint, using a measurement at two different points of the joint; specifically, a measurement point is taken at each side of the elbow, Figure 4. This measurement system makes it possible to quantify the range of movement (ROM) of the joint.

Figure 4. Photographs of the wearable device worn by the user. Left: extension of the elbow junction, close to 0 degrees angle, calibration position; right: flexion at an approximation of 90 degrees
In essence, the hardware part of the system consists of two different components, and their combination enables the functionality of the device. The central node is the core of the system and the satellite node performs as a slave of the central one. Both of them are represented in Figure 5. In addition, the photographs in Figure 4 show their appearance when installed on the wearable sleeve.
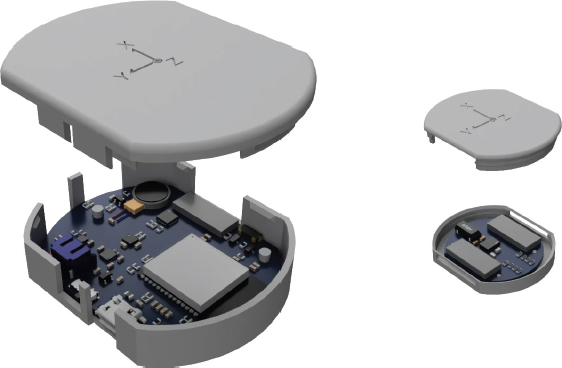
Figure 5. 3D representation of the central and satellite nodes. Left: central node, the battery is placed between the PCB and the lid; right: satellite node
From the measures taken by the central node and the satellite node, the logic programmed in the device calculates the position of the elbow joint, and, thus, the range of mobility after the processing. This architecture allows to take the relevant elbow rotation and flexion measurements, which is, basically, the raw material to analyse, visualise and take customised decisions in the telerehabilitation platform. As it will be explained further in this section, both devices integrate a nine-axis inertial measurement unit (IMU). The low level architecture is depicted in Figure 6 where there is a central part based on a microcontroller which manages the entire system. The IMUs presented are in charge of taking the data to be processed in order to calculate the ROM; all the data is sent through BLE to the gateway and, at the end, to the cloud platform.
Central Node
This is the smart part of the IoT system, which is in charge of the management of all the integrated hardware, and it also includes all the subsystems of any complete IoT device: power, processing, communications, sensors and user interface. This part is shown on the left side of Figure 5, and it is conceived as the Master. In addition, the central node is one of the measurement points as it has an integrated nine-axis IMU.
Regarding the power, this part includes the battery, the charger and the management to ensure a stable and efficient power delivery to all the different components. The communication part, which is made via BLE, allows the data to be sent to the app, which acts as a gateway. The IMU sensor is connected through I2C and, in order to admit more than one sensor, an I2C multiplexer is used; it also has a connector that permits the cascaded connection of multiple satellite devices. The user interface is reduced to the minimum, it only has one button for switching the device on and off, and a multi-colour led that shows the state of the system. Finally, the processing part, which is composed by an ESP32 microcontroller, orchestrates data processing and communication flow within the system. As shown in Figure 4, the central node is placed on the arm, just above the elbow joint.

Figure 6. Architecture and technical diagram of the wearable IoT device
Satellite Node
The satellite node is a slave device, which is connected through a wire to the master, and it works as a peripheral part of the central node. This slave device is presented on the right side of Figure 5.
This part is much simpler than the central node. It is mainly composed by a nine-axis IMU, whose measures can be combined with the ones taken in the central node. As it was shown in Figure 4, the satellite node is placed on the forearm, just below the elbow junction.
Mechanical
In terms of mechanical design, the aforementioned parts have been adapted ergonomically to a fabric sleeve, see Figure 4. For this purpose, a different package has been designed for each of the described elements. This has been done to enable the placing of the wearable over the joint. To make the wearable washable which means that the electronic part should be removable, a Velcro tape has been used; thus, a strap is knitted to the sleeve, and the complementary part is glued to the bottom of the enclosure.
3.7. Firmware and Calibration
Regarding the firmware integrated in the wearable device, as mentioned above, all the intelligence is integrated in an ESP32 microcontroller with BLE connectivity. In this way, the angle of the joint is calculated by the combination of the value readings of two accelerometers, strategically placed in the wearable device.
Each of the accelerometers defines its own location on the basis of its initialisation conditions. It is important, at the starting time, for the arm to be in extension position, approximately, at 0 degrees of elbow flexion, so that the reference points can be taken correctly, (Madgwick et al., 2010). As the elbow has an additional degree of freedom, pronation and supination movements, a transformation of the position of the sensor placed on the forearm is necessary if it is not in the same plane during the calibration process, see Figure 7.
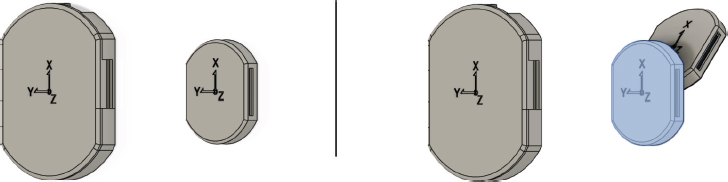
Figure 7. Representation of the initialisation process of the two sensors. Left: no transformation; right: rotation and lateral movement transformation
The diagram on the left of Figure 7 shows an initialisation condition in which the two sensors, represented in grey, are aligned on the same plane, and no transformation is necessary. On the other hand, the right side of Figure 7 shows the lateral movement and rotation that is necessary if the initialisation were performed with incorrectly aligned sensors, which are represented in grey. In this manner, the position of the forearm sensor is rotated and translated until it allows for the correct operation of the joint measurement, represented in blue. In the event that the calibration process is incorrect, and anomalous measurements are taken, a new calibration can be performed using the mobile application or just by restarting the device. Thus, as the operations are made in quaternions just to reduce computational cost and avoid the ambiguity of Euler angles representation, (Miron et al., 2023). The calibration rotation and initialisation could be done through the operation (1), where p represents the original quaternion, q is defined as the quaternion that is the initialisation rotation (2) and q-1 is the inverse quaternion. The rotation is mainly done in the y-axis as the pronation/supination of the arm produces this movement, it also takes into account the forearm radius and the θ angle is defined as the initial angle between the hardware devices. In order to calculate θ, the initial position of each device should be processed within the initial axis on each device.
Thus, once the calibration has been performed, a continuous monitoring of the angle formed by the joint is initiated. As the device is initialised aligned with the elbow, the joint angle could be calculated (3), as the equation between two quaternions where p1 and p2 are the quaternions of interest and ϕ is the angle between them. In this way, measurements are taken for as long as the user has the device in place and, in particular, during the process of taking samples for the clinical follow-up of the app. The conversion between quaternions and Euler angles can be made computationally efficient, (Bernardes and Viollet, 2022).
Finally, in order to summarise the algorithm for calculating the ROM within the angles and the representation made in the application, a pseudo code sequence is presented on Algorithm 1.
Algorithm 1 Sequence of operation within the wearable
Require: Initialisation of sensors
Ensure: Calibration
Calculate relative position between sensors, θ
⊳ Sensors data: quaternions
while θ is defined do
Rotate the sensor position w/ θ, equation (1) and (2)
Calculate the joint angle, ϕ, equation (3)
Convert to Euler
Send information
⊳ Processed data: ϕ, quaternions and Euler representation
end while
4. Results
The completion of this project has resulted in the deployment of the proposed tele-rehabilitation system. This system is mainly based on software, and it allows for the active, exhaustive and remote monitoring of the evolution of the patient’s joint lesion recovery.
The developed system is based on three main elements: the tele-rehabilitation web platform, the IoT wearable device for the elbow and the mobile application, which is the link between the aforementioned two parts. This set has been tested at a clinical level in the University Hospital of Salamanca and different results have been obtained at the component level.
4.1. Integration Plan
From a functional perspective, the system has been designed to minimise its impact on the working methods of healthcare personnel. The device collects data on patients’ rehabilitation path, therefore, also the recovery process, and the platform enables healthcare professionals to visualize this data, serving as support for decision-making. However, this system does not alter the treatments or rehabilitation techniques known to healthcare personnel, but, additionally, it helps with the decision making.
Simplicity and accessibility to all its functionalities have been the main objectives during the design and development with the aim of smoothing the learning curve. As shown in Figure 3, a main menu providing access to all system functionalities is included on the landing page with descriptive icons for each functionality and contrasted colors. This minimalist and intuitive design makes easier the acceptance among healthcare professionals, as a more friendly and easy-to-understand environment is presented.
Despite the simplicity-oriented design, it is crucial to consider a gradual integration into hospitals and rehabilitation centers until it becomes a routine tool. Following these guidelines, a collaboration with the Trauma and Orthopedic Surgery team at the University Hospital of Salamanca has been put into practice; receiving feedback and iterating on functionality to enhance the system’s operability by means of tests conducted by volunteers.
In order to evaluate the system, a set of 10 key parameter indexes (KPIs) has been created; they are defined in Table 7. Thus, with the use of these parameters, the evaluation of the tele-rehabilitation environment (wearable, mobile app and web platform) is made, taking into account all the parts defined on the architecture all together. These KPIs allow for the comparison between the already established methods and the paradigm enabled with the tele-rehabilitation system proposed in this work.
Table 7. List of the defined KPIs. This set of parameters allows for objective evaluation of the proposed tele-rehabilitation system
Parameter |
Definition |
Time to measure |
The time that a healthcare professional or the patient himself lasts to make an acceptable measurement. |
Accuracy |
The degree of correctness of the taken measurement. |
Repeatability |
The quality of giving the same value to different consecutive measures of the same fact. |
Frequency of use |
The times the device is used. |
Time of goal achievement |
The time needed to achieve different goals during the recovery. |
Reduction on Hospital visits |
The reduction on the number of visits to the Hospital taking into account the information collected by the healthcare professionals. |
Convenience |
The comfortableness of the system for the user. |
Time to recovery |
The time to the recovery following the rehabilitation path with the system. |
Abandon rate for patients |
The percentage of patients that left the rehabilitation process. |
Abandon rate for professionals |
The percentage of professionals that left the use of the system in the rehabilitation process they diagnose and follow. |
4.2. Wearable Device
The wearable device, as it has been presented, is an IoT device. This element is the interface of the system, i.e., the connection between the physical data and the IT elements. In the conducted tests, accurate and repeatable measurements of the patients’ joints have been obtained. These measurements have been assessed using a goniometer, which is a widely used tool in orthopaedic and physiotherapy, and the results have revealed that the developed wearable is a powerful and reliable tool for monitoring the joint’s range of mobility. The IoT solution has fulfilled its purpose; it obtains clinically useful and more precise data than previous state-of-the-art tools, whose results were affected by the subjectivity of the clinical staff in charge of the task. The first tests took place with volunteers and the results are summarised in table Table 8. These volunteers had been diagnosed with injuries or they had suffered different surgeries. Thus, after the initialisation of the system, the user is requested to move his/her arm and, then, the measures were taken with the arm stretched and with the maximum flexion the user was able to achieve actively. At this point of the study, the validation of the device is the main purpose of the tests, so the clinical person in charge of taking the measures with the goniometer is blinded to the results provided by the wearable.
Table 8. Measures of range of motion (ROM) with the wearable compared with the manual goniometer within volunteers. Minimum and maximum, i.e., flexion and extension angles in degrees are shown
# |
Injury |
Goniometer |
Wearable |
1 |
Humeral fracture |
14 - 120 |
14.6 - 119.6 |
2 |
Post-traumatic stiffness |
23 - 125 |
24.5 - 126.7 |
3 |
Post-traumatic stiffness |
14 - 110 |
14.7 - 108.3 |
4 |
Post-traumatic stiffness |
19 - 117 |
18.9 - 118.9 |
5 |
Humeral fracture |
20 - 100 |
21.1 - 98.7 |
6 |
Control subject |
-1 - 142 |
-0.8 - 143.2 |
7 |
Control subject |
0 - 135 |
-0.2 - 136.4 |
8 |
Control subject |
-1 - 140 |
0 - 138.7 |
9 |
Control subject |
0 - 145 |
0 - 143.4 |
10 |
Control subject |
-2 - 140 |
-1.5 - 141.2 |
As it is shown in Table 8, the differences between the goniometer and the wearable have not any clinical significance. Furthermore, the results present that the device is reliable and, with their use, doctors could take objective measures not based on the skills with a tool.
4.3. Mobile App
The mobile application is a key component of the system, and it is designated for patient data acquisition. As it has been stated in the previous sections, this component effectively bridges the data gap between the physical joint measurement device and the web data platform, as the digitisation of data is essential to enable the active and remote monitoring of a recovering patient. All the collected data is sent to the cloud and stored in the database; the data includes questionnaire responses filled by the patient, the recorded wearable device information, and, also, pictures that, for instance, depict the state of the surgery wounds.
The most important factor of the mobile app is that it displays the evolution of elbow joint mobility, which helps patients to visualise their rehabilitation path. The communication between the wearable and the app, which is based on BLE, has proven effective.
Patients have positively rated the interface of the app and its overall functionality. Their reports point to the intuitiveness of the app and to its effective and motivational role in the recovery process. Additionally, it enables the patient to interact with the clinical staff remotely, reducing the need for time-consuming follow-up visits in person.
4.4. Web Platform
The web platform, as it is oriented for use by clinical staff and administrators, can be described as the main clinical part of the system. The platform is designated for the follow-up and evaluation of the patients, and positive reports have been collected from the doctors and orthopaedic specialists involved in the testing of the platform. It has been categorised as a useful tool form of remote patient management and a perfect telerehabilitation environment.
The platform allows for the remote monitoring of patients and provides the functionalities required to guide them in their recovery, including personalised alerts, advice, and goals that motivate them along the process. All of these elements are sent to the patient’s application, along with the custom questionnaires adapted to each user.
Additionally, the platform constitutes a data centralisation tool, which enables massive data analysis and comparative studies with the aim of predicting the evolution of the injuries. In the near future, this data analysis could be adapted to take into account different pathologies, ages or rehabilitation techniques, among others, so as to make the tool more complete, ensuring optimal patient recovery.
4.5. Discussion
The initial testing with volunteers demonstrated the effectiveness of the wearable in capturing elbow joint range mobility data. The device’s design has facilitated its use and integration in the rehabilitation process, as it is easy to wear and can be adapted to each person; a conventional orthosis can be worn at the same time. Notably, the device, in conjunction with the mobile app, accurately recorded the range of motion of the elbow joint, aligning with, or even improving, manual measurements. The comparative analysis between manual goniometer measurements and the device’s data revealed minor discrepancies, but these were within acceptable clinical margins. This validation underscores the device’s accuracy and unbiased reliability in monitoring the rehabilitation progress. At this point, the device has been evaluated taking into account the KPIs defined in Table 7, and the results after the test with 5 patients are summarised in Table 9.
Table 9. List of values for the evaluated KPIs in the preliminar tests with patients
Parameter |
Value for the system |
Time to measure |
3 seconds. |
Accuracy |
±3 degrees. |
Repeatability |
±0.1 degrees. |
Frequency of use |
Three times a week. |
Time of goal achievement |
One week - Depending on how ambitious the goal was. |
Reduction on Hospital visits |
Three times less visits. |
Convenience |
Complete satisfaction. |
Time to recovery |
It is reduced by a third. |
Abandon rate for patients |
No abandon. |
Abandon rate for professionals |
No abandon. |
As shown in Table 9, although there is some time to obtain a stable measure, the time to get a valid ROM is too low for each position (maximum and minimum extension) and, also, it is much lower than the time taken using the manual goniometer. Additionally, the accuracy is high enough for clinical purposes, independent of the user skills with a tool and the repeatability of the measures is higher with the system than it could be with an interpreted tool. Following the indications of the healthcare professionals, the use of the device for taking measures could be three times a week for measuring the ROM, but the recommendation for completing the questionnaires is once a week, which improves the follow-up as the patient would be seeing the doctors that regularly; this justifies the reduction of the visits to the Hospital as the injury has a more intensive tracking and, even, the regular consultations can be reduced due to the nature of telerehabilitation. The patients have pointed out that the system is convenient as their recovery accelerates due to the instant feedback and they have no need to go to the doctors for examination. Also, the feedback has been reported by both patients and professionals as a means of achieving the goals, which leads to a faster recovery. After the preliminary test, the recovery time has been reported to be a third less than the estimated recovery time with the standard rehabilitation path. At the time being, there have not been reports for abandoning the telerehabilitation system nor the existence of dissatisfaction.
The implementation of customised questionnaires sent to the patient through the mobile app, has been successfully accepted, with patients easily accessing and completing them. The inclusion of multiple-choice questions, open-ended queries, and the Visual Analog Scale (VAS) for pain assessment, among other aspects related to the patient’s perceptions, has provided a comprehensive tool for evaluating patient status, taking into account the patient’s concerns. The positive reception of these questionnaires by both the clinical staff and the patients highlights their effectiveness and user-friendliness.
It can be concluded, therefore, that the developed tele-rehabilitation system is useful for both professionals in the health sector, specifically orthopaedic surgeons and physiotherapists, and for patients. The system allows for the personalised, continuous, and remote monitoring of each patient, enabling a close follow-up and an early response to the anomalies that could arise in the recovery process.
4.6. Motivation and Justification of this Work
Elbow injuries, prevalent in a variety of sports, pose a significant challenge to athletes’ performance and the longevity of their careers. Traditional rehabilitation methods, while somewhat effective, often lack the precision and personalisation necessary to fully meet athletes’ recovery needs. Recognizing this gap, our research introduces an innovative solution that leverages advancements in wearable technology and tele-rehabilitation platforms. This novel approach is embodied in a device equipped with advanced sensors, capable of providing real-time, precise tracking of elbow joint movements. Integrated with a comprehensive tele-rehabilitation platform, which includes both a mobile application and a web interface, this system marks a significant leap in the rehabilitation process.
Our findings reveal marked improvements in the accuracy and effectiveness of rehabilitation strategies, offering personalized plans informed by real-time feedback. When compared with conventional methods, our system demonstrates superior performance in accuracy, adherence to rehabilitation protocols, and the speed of recovery. This study not only highlights the system’s immediate benefits for sports medicine but also its broader implications for healthcare, suggesting a shift towards more personalized, data-driven care.
The development of this system responds to the urgent need for more sophisticated rehabilitation strategies that harness the potential of cutting-edge technologies. By filling the existing void in rehabilitation practices with a solution that offers real-time monitoring and comprehensive data analysis, we facilitate a more personalized and effective recovery process. This approach not only promises enhanced recovery outcomes but also aligns with the evolving landscape of data-driven, patient-centered healthcare.
Furthermore, a comparative analysis with traditional rehabilitation methods underscores our system’s potential to significantly refine current practices, emphasizing its contributions not just to sports medicine, but to the wider field of healthcare. The potential of this methodology to manage chronic musculoskeletal conditions extends its applicability beyond sports-related injuries, underlining the system’s relevance in a broader healthcare context. At its core, this work is driven by the goal of improving patient outcomes, elevating the quality of care, and pushing the boundaries of rehabilitation through technological innovation.
5. Conclusions
This study has made significant contributions to the field of sports medicine, particularly in enhancing the rehabilitation process for elbow injuries. It has successfully achieved its research goals by integrating innovative medical technologies into practical solutions. The development has been centred on the deployment of a tele-rehabilitation platform aimed at improving the evaluation and clinical follow-up of the patients.
A major achievement of this research is the development of a wearable device designed for the precise measurement of elbow joint mobility in real time. This device, equipped with advanced sensor technology, marks a paradigm shift in monitoring Range of Motion (ROM), offering critical data to athletes and rehabilitation patients. Its real-time feedback capability is a key factor in ensuring an effective and closely monitored recovery processes.
Additionally, the creation of a mobile application for data management and visualisation significantly enriches the rehabilitation experience. This app not only tracks physical parameters in real time but also includes functionalities such as session tracking, expert advice, and telemedicine options. It stands out for its ease of use and for empowering patients to play an active part in their own recovery process.
The inclusion of customisable forms in the app represents a tailored approach to patient care, crucial for tracking individual progress. These forms have been seamlessly integrated into the app and web platform system, simplifying the process of remote monitoring, and enhancing patient care efficiency. A sophisticated data visualisation interface has been developed to provide a detailed and clear view of patient progress. This tool is invaluable to healthcare professionals, enabling them to make well-informed decisions and offer a higher quality of care by presenting a comprehensive view of the patient’s rehabilitation path.
The system’s effectiveness and reliability have been validated through extensive testing and real-world application. This comprehensive testing, meeting specific evaluation criteria, not only confirms the theoretical foundations of the project but also its practical applicability, promoting medical tele-rehabilitation scenarios. Several tests have been carried out to validate the measures made with the use of the wearable reporting useful clinical values. Additionally, a set of 10 KPIs has been defined in order to validate the tele-rehabilitation system; these parameters are established with a focus on the rehabilitation path and its success, taking into account aspects relative to both the patients and the health care professionals.
In summary, this research has successfully met its objectives, contributing significantly to the advancement of medical technology in the field of elbow rehabilitation, in particular tele-rehabilitation. The combination of cutting-edge wearable devices, a patient-oriented mobile app, and an efficient data management system forms an innovative approach in monitoring and aiding patient recovery. This achievement not only validates the current system but also sets the stage for further innovations in the broader field of sports medicine and orthopaedics.
The system’s visualisation feature, which graphically displays elbow mobility data within the app, has been particularly effective in enhancing patient engagement and aiding healthcare professionals in providing precise, personalised care. The system simplifies data gathering for both patients and medical professionals by integrating various data types such as questionnaires, visual analog scale (VAS) data, device measurements, and photographs, thus improving the management of clinical data and healthcare communication.
Future enhancements could include adapting sensor technology to smaller devices, such as flexible bands or patches, providing patients with more comfort and freedom during their recovery, especially in cases of less severe injuries. Such improvements would focus on tailoring the technology to individual patient needs and comfort, further advancing the field of personalised medical care.
Funding
The development of the project «InTrack - Intelligent tracking of articulations in recently operated athletes», with reference EXP_75058, has been financed within the framework of the Call for Grants for research projects in science and technology applied to physical activity for health (AFBS) and sports medicine under the European Funds of the Recovery, Transformation and Resilience Plan - NextGenerationEU, managed by the Consejo Superior de Deportes (Spain) in its role of promoting institution.
Consent
Informed consent was obtained from all subjects involved in the study.
Acknowledgments
This research has been supported by the project «InTrack - Intelligent tracking of articulations in recently operated athletes», with reference EXP_75058.
References
Ali, N. M., Sing, G., Yee, C., Kang, T., Chee, T., Ab Rashid, M., Sulaiman, M., Razi, A., Hasan, Z., & Abidin, A. (2018). A review of different applications of wireless sensor network (WSN) in monitoring rehabilitation. Journal of Telecommunication, Electronic and Computer Engineering (JTEC), 10(1-9), 121–127.
Bernardes, E., & Viollet, S. (2022). Quaternion to Euler angles conversion: A direct, general and computationally efficient method. PLoS One, 17(10), e0276302. https://doi.org/10.1371/journal.pone.0276302
Brookshaw, M., Sexton, A., & McGibbon, C. A. (2020). Reliability and validity of a novel wearable device for measuring elbow strength. Sensors, 20(12), 3412. https://doi.org/10.3390/s20123412
Cardinale, M., & Varley, M. C. (2017). Wearable training-monitoring technology: applications, challenges, and opportunities. International Journal of Sports Physiology and Performance, 12(s2), S2–55.
Del Din, S., Patel, S., Cobelli, C., & Bonato, P. (2011). Estimating Fugl-Meyer clinical scores in stroke survivors using wearable sensors. In 2011 Annual International Conference of the IEEE Engineering in Medicine and Biology Society (pp. 5839–5842). IEEE.
Faisal, A., Majumder, S., Mondal, T., Cowan, D., Naseh, S., & Deen, M. (2019). Monitoring Methods of Human Body Joints: State-of-the-Art and Research Challenges. Sensors, 19(11), 2629.
Fennema, M., Bloomfield, R., Lanting, B., Birmingham, T., & Teeter, M. (2019). Repeatability of measuring knee flexion angles with wearable inertial sensor. The Knee, 26(1), 97–105.
Fusaro, I., Orsini, S., Stignani Kantar, S., Sforza, T., Benedetti, M., Betteli, G., & Rotini, R. (2014). Elbow rehabilitation in traumatic pathology. Musculoskeletal Surgery, 98(Suppl 1), 95–102.
Greco, F., Bandodkar, A. J., & Menciassi, A. (2023). Emerging technologies in wearable sensors. APL Bioengineering, 7(2).
Guk, K., Han, G., Lim, J., Jeong, K., Kang, T., Lim, E.-K., & Jung, J. (2019). Evolution of wearable devices with real-time disease monitoring for personalized healthcare. Nanomaterials, 9(6), 813.
Hadjidj, A., Souil, M., Bouabdallah, A., Challal, Y., & Owen, H. (2013). Wireless sensor networks for rehabilitation applications: Challenges and opportunities. Journal of Network and Computer Applications, 36(1), 1–15.
Hristov, S. (2023). Wearables & Lifestyle: Wearables & Stress. B.S. thesis, University of Twente.
Höher, J., Lischke, B., Petersen, W., Mengis, N., Niederer, D., Stein, T., Stoffels, T., Prill, R., & Schmidt-Lucke, C. (2023). Sensor-based telerehabilitation system increases patient adherence after knee surgery. PLOS Digital Health, 2(2).
Huanan, Z., Suping, X., & Jiannan, W. (2021). Security and application of wireless sensor network. Procedia Computer Science, 183, 486–492. https://doi.org/10.1016/j.procs.2021.02.088
Idoudi, M., Bourennane, E.-B., & Grayaa, K. (2018). Wireless visual sensor network platform for indoor localization and tracking of a patient for rehabilitation task. IEEE Sensors Journal, 18(14), 5915–5928.
Johnston, M. V., & Dijkers, M. P. (2012). Toward improved evidence standards and methods for rehabilitation: recommendations and challenges. Archives of Physical Medicine and Rehabilitation, 93(8), S185–S199.
Kastoriano, I., & Halkias, D. (2020). Applying the technology adoption model (TAM) to explore consumers’ perceptions of wearable technology: a multiple case study of an ironman triathlon community: a narrative literature review. Available at SSRN 3637423.
Kim, J. Y., Park, G., Lee, S. A., & Nam, Y. (2020). Analysis of machine learning-based assessment for elbow spasticity using inertial sensors. Sensors, 20(6), 1622. https://doi.org/10.3390/s20061622
Kliethermes, S. A., Nagle, K., Côté, J., Malina, R. M., Faigenbaum, A., Watson, A., Feeley, B., Marshall, S. W., LaBella, C. R., Herman, D. C., et al. (2020). Impact of youth sports specialisation on career and task-specific athletic performance: a systematic review following the American Medical Society for Sports Medicine (AMSSM) Collaborative Research Network’s 2019 Youth Early Sport Specialisation Summit. British Journal of Sports Medicine, 54(4), 221–230.
Li, R. T., Kling, S. R., Salata, M. J., Cupp, S. A., Sheehan, J., & Voos, J. E. (2016). Wearable performance devices in sports medicine. Sports Health, 8(1), 74–78.
Madgwick, S., et al. (2010). An efficient orientation filter for inertial and inertial/magnetic sensor arrays. Report x-io and University of Bristol (UK), 25, 113–118.
McGibbon, C. A., Sexton, A., Jones, M., & O’Connell, C. (2013). Elbow spasticity during passive stretch-reflex: clinical evaluation using a wearable sensor system. Journal of Neuroengineering and Rehabilitation, 10(1), 1–14.
Meijer, H. A., Graafland, M., Goslings, J. C., & Schijven, M. P. (2018). Systematic review on the effects of serious games and wearable technology used in rehabilitation of patients with traumatic bone and soft tissue injuries. Archives of Physical Medicine and Rehabilitation, 99(9), 1890–1899.
Miron, S., Flamant, J., Bihan, N. L., Chainais, P., & Brie, D. (2023). Quaternions in Signal and Image Processing: A comprehensive and objective overview. IEEE Signal Processing Magazine, 40(6), 26–40. https://doi.org/10.1109/MSP.2023.3278071
Morris, D. M., Uswatte, G., Crago, J. E., Cook III, E. W., & Taub, E. (2001). The reliability of the wolf motor function test for assessing upper extremity function after stroke. Archives of Physical Medicine and Rehabilitation, 82(6), 750–755.
Nuevo, M., Mahdavi, H., Rodríguez, D., Faura, T., Fabrellas, N., Balocco, S., Conti, M., Castagna, A., & Prat, S. (2021). Evaluation of Safety and Efficacy of ReHub in Patients Who Underwent Primary Total Knee Arthroplasty: Study Protocol for a Randomized Controlled Trial. International Journal of Surgery Protocols, 25(1), 34–41.
Oosterwijk, A., Nieuwenhuis, M., van der Schans, C., & Mouton, L. (2018). Shoulder and elbow range of motion for the performance of activities of daily living: A systematic review. Physiotherapy Theory and Practice, 34(7), 505–528.
Ozel, O., & Demircay, E. (2016). Review of management of unstable elbow fractures. World Journal of Orthopedics, 7(1), 50–54.
Preatoni, E., Bergamini, E., Fantozzi, S., Giraud, L. I., Orejel Bustos, A. S., Vannozzi, G., & Camomilla, V. (2022). The use of wearable sensors for preventing, assessing, and informing recovery from sport-related musculoskeletal injuries: a systematic scoping review. Sensors, 22(9), 3225.
Rahman, S. M., Ali, M. A., & Al Mamun, M. A. (2021). The use of wearable sensors for the classification of electromyographic signal patterns based on changes in the elbow joint angle. Procedia Computer Science, 185, 338–344. https://doi.org/10.1016/j.procs.2021.01.188
Rigamonti, L., Albrecht, U.-V., Lutter, C., Tempel, M., Wolfarth, B., Back, D. A., et al. (2020). Potentials of digitalization in sports medicine: a narrative review. Current Sports Medicine Reports, 19(4), 157–163.
Rodgers, M. M., Alon, G., Pai, V. M., & Conroy, R. S. (2019). Wearable technologies for active living and rehabilitation: Current research challenges and future opportunities. Journal of Rehabilitation and Assistive Technologies Engineering, 6, 2055668319839607.
Rose, M., Curtze, C., O’Sullivan, J., El-Gohary, M., Crawford, D., Friess, D., & Brady, J. M. (2017). Wearable inertial sensors allow for quantitative assessment of shoulder and elbow kinematics in a cadaveric knee arthroscopy model. Arthroscopy: The Journal of Arthroscopic & Related Surgery, 33(12), 2110–2116. https://doi.org/10.1016/j.arthro.2017.06.033
Ryan, M., Kinghorn, P., Entwistle, V. A., & Francis, J. J. (2014). Valuing patients’ experiences of healthcare processes: towards broader applications of existing methods. Social Science & Medicine, 106, 194–203.
Schuberg, I., Strohm, P., Maier, D., & Zwingmann, J. (2021). Simple traumatic elbow dislocations; benefit from early functional rehabilitation: A systematic review with meta-analysis including PRISMA criteria. Medicine, 100(44), e27168.
Seçkin, A. Ç., Ateş, B., & Seçkin, M. (2023). Review on wearable technology in sports: Concepts, challenges and opportunities. Applied Sciences, 13(18), 10399.
Segura Anaya, L., Alsadoon, A., Costadopoulos, N., & Prasad, P. (2018). Ethical implications of user perceptions of wearable devices. Science and Engineering Ethics, 24, 1–28.
Seron, P., Oliveros, M., Gutierrez-Arias, R., Fuentes-Aspe, R., Torres-Castro, R., Merino-Osorio, C., Nahuelhual, P., Inostroza, J., Jalil, Y., Solano, R., Marzuca-Nassr, G., Aguilera-Eguía, R., Lavados-Romo, P., Soto-Rodríguez, F., Sabelle, C., Villarroel-Silva, G., Gomolán, P., Huaiquilaf, S., & Sanchez, P. (2021). Effectiveness of telerehabilitation in physical therapy: A rapid overview. Physical Therapy, 101(6), 1–18.
Seshadri, D. R., Rowbottom, J. R., Drummond, C., Voos, J. E., & Craker, J. (2016). A review of wearable technology: Moving beyond the hype: From need through sensor implementation. In 2016 8th Cairo International Biomedical Engineering Conference (CIBEC) (pp. 52–55). IEEE.
Zadeh, A., Taylor, D., Bertsos, M., Tillman, T., Nosoudi, N. & Bruce, S. (2021). Predicting sports injuries with wearable technology and data analysis. Information Systems Frontiers, 23, 1023 - 1037. https://doi.org/10.1007/s10796-020-10018-3